Featured
- Get link
- X
- Other Apps
Cobra Continuation Of Coverage Application
In order to continue your coverage you must fill out an Application and Election Form. COBRA establishes required periods of coverage for continuation health benefits.
Https Www Mass Gov Doc Cobra Aei Application Download
You may use the special enrollment period to enroll in Marketplace coverage with a tax credit if you end your COBRA continuation coverage when your premium assistance ends and you are otherwise eligible.

Cobra continuation of coverage application. Deadline if the individual fails to pay any amount towards the total premiums due for periods of retroactive COBRA continuation coverage the employer may treat the individual as having not elected COBRA coverage until the first period of coverage. 9501a1 for the quarter. Application of Emergency Relief Notices to payment of premiums for retroactive coverage QA 58.
To elect COBRA continuation of health coverage the eligible person must complete a COBRA - Continuation of Coverage Application. To elect COBRA continuation of health coverage the eligible person must complete a COBRA - Continuation of Coverage Application. Application for Continuation of.
If you elect COBRA continuation coverage with premium assistance then you may qualify for a special enrollment period to enroll in Marketplace coverage when your premium assistance ends. Both you and your dependents should take the time to read that section carefully. Marketplace or conversion coverage is available without a waiting period for preexisting conditions.
Are required to offer employees and dependents losing eligibility the option to continue their coverage. This notice provides guidance on the application of 9501 of the American Rescue Plan Act of 2021 the ARP Pub. A plan however may provide longer periods of coverage beyond those required by COBRA.
In general under COBRA an individual who was covered by a group health plan on the day before the occurrence of a qualifying event such as a termination of. The coverage and premium amount may vary greatly from plan to plan. Extension of the 60-day election period for COBRA continuation coverage.
COBRA continuation coverage provides certain group health plan continuation coverage rights for participants and beneficiaries covered by a group health plan. SCMEBF Continuation of Coverage COBRA Application If you are an eligible member of the Benefit Fund who recently retired or separated from employment you may continue full-coverage for a limited time through a federally mandated offering known as COBRA the Consolidated Omnibus Reconciliation Act. Employees andor eligible family members can obtain application forms from their agency payroll or personnel office.
In this case the amount of the premiums not paid by the AEI is the premium amount charged for COBRA. As required by law you are eligible to apply for Marketplace or conversion coverage when group continuation coverage terminates. Review the COBRA Continuation Coverage Election package.
If you wish to extend coverage you must complete this form and. Click Next to be taken to the Online Form. Please contact the welfare fund if you wish to.
4 March 11 2021 relating to temporary premium assistance for Consolidated Omnibus Budget Reconciliation Act of 1985 COBRA continuation coverage. If the employer does not subsidize COBRA premium costs for similarly situated qualified beneficiaries who are not AEIs the credit for a quarter is the amount equal to the premiums not paid by AEIs for COBRA continuation coverage due to the application of ARPA Sec. Applicant is requesting continuation of coverage pursuant to COBRA due to the following reason check applicable box.
Employees andor eligible family members can obtain application forms from their agency payroll or personnel office. This section provides additional information about continuation coverage. COBRA beneficiaries generally are eligible for group coverage during a maximum of 18 months for qualifying events due to employment termination or reduction of hours of work.
Certain qualifying events or a second qualifying event during the initial period of coverage. Section 9501 of the ARP COBRA Premium Assistance. Group Vision Coverage COBRA With the passage of the Consolidated Omnibus Budget Reconciliation Act of 1985 COBRA most employer-sponsored group health plans.
If you terminate your COBRA continuation coverage. Your COBRA continuation rights are described in the FederalState Notifications section online. Please contact the welfare fund if you wish to purchase its benefits.
Contact the plan directly to make application for coverage. Upon receiving notification of their COBRA rights eligible. Submit the completed and signed COBRA Enrollment Form to the Employee Benefits Administration Office no later than 60 days after City of Mesa coverage ends or within 60 days of the date of the COBRA Election package notification whichever is later.
Continued coverage for a maximum of eighteen 18 months due to employees reduction in work hours retirement or termination on. The employee and his or her family members may each elect to continue health coverage under COBRA request the premium assistance. Steps to elect COBRA coverage.
You do not have to provide evidence of insurability to enroll in continuation coverage. COBRA Continuation Coverage. The applicant person requesting review of a denial of premium assistance may either be the former employee or a member of the employees family who is eligible for COBRA continuation coverage or the COBRA premium assistance through an employment-based health plan.
Https Www Anthem Com Agent Co F5 S2 T0 Pw A073582 Pdf Refer Ahpfooter
 Employers Now Required To Pay 100 Of Cobra Premiums
Employers Now Required To Pay 100 Of Cobra Premiums
Cobra Continuation Coverage Rights General Notice California Employees Hrcalifornia
Https Www Blueshieldca Com Bsca Bsc Public Broker Portalcomponents Streamdocumentservlet Filename C11825 Rtm Ff 10 16 Pdf
Https Www Birminghamal Gov Wp Content Uploads 2020 08 Cobra Packet City Of Birmingham Pdf
Http Sageba Com Wp Content Uploads 2010 02 Anthem Cont Form Pdf
Https Www Dol Gov Sites Dolgov Files Ebsa About Ebsa Our Activities Resource Center Faqs Cobra Continuation Health Coverage For Employers Pdf
Https Www Bcbstx Com Pdf Forms Grp Cobra Continuation Tx Pdf
Https Www Bcbstx Com Pdf Forms Grp State Continuation 6mo Tx Pdf
Https Oci Wi Gov Documents Consumers Pi 023 Pdf
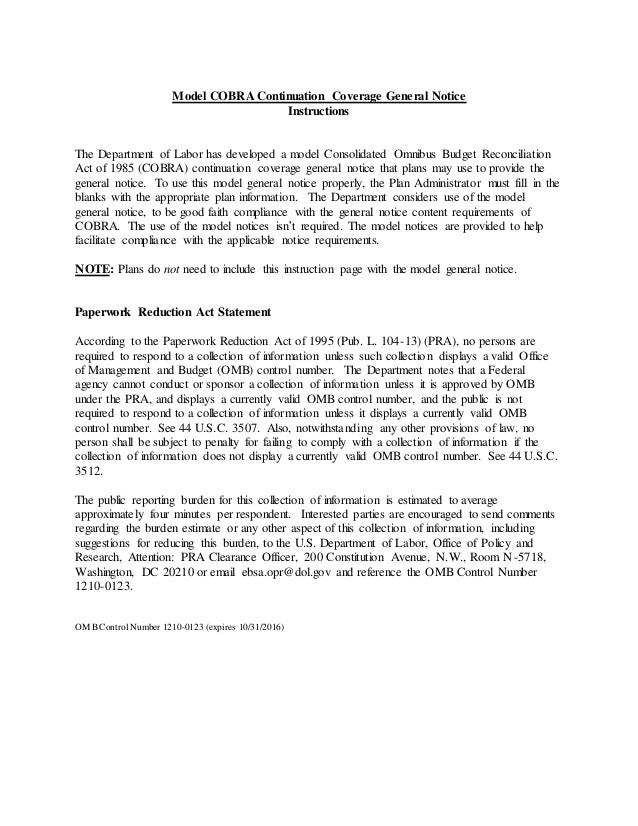 Model Cobra Continuation Coverage General Notice
Model Cobra Continuation Coverage General Notice
Comments
Post a Comment