Featured
- Get link
- X
- Other Apps
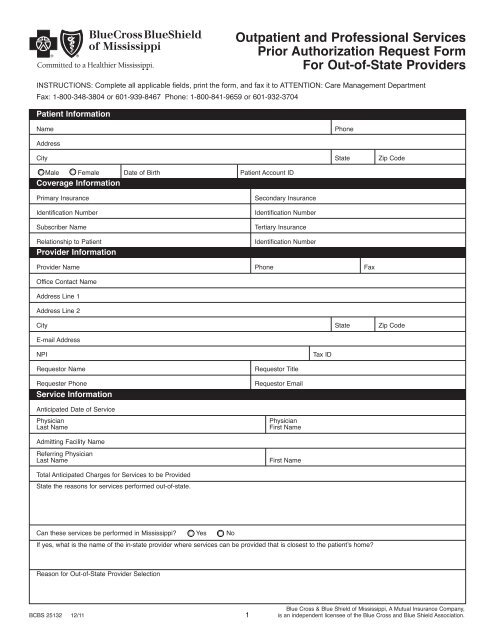
Bcbs Of Mississippi Prior Authorization Form
Behavioral Health Substance Abuse Certification. Prior Authorization A process that allows physicians and other professional providers to determine before treating a patient if Blue Cross Blue Shield of Michigan will cover the cost of a proposed service.
 Mississippi Bcbs Form Fill Out And Sign Printable Pdf Template Signnow
Mississippi Bcbs Form Fill Out And Sign Printable Pdf Template Signnow
You can download the Physician Request for Prior Authorization form also called the Formulary Exception form.
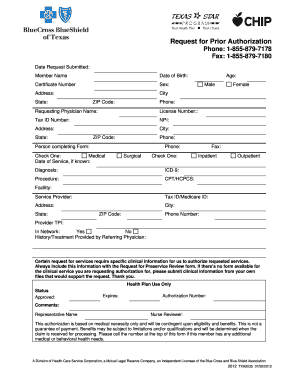
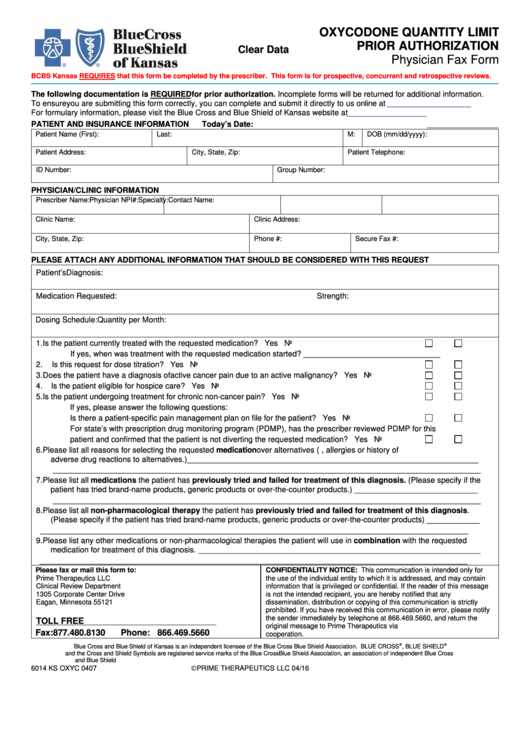
Bcbs of mississippi prior authorization form. Office drugs prior authorization request PDF 301 KB Home Self-Administered Injectable Drug authorization request PDF 288 KB. Enhanced Personal Health Care. Focused Outpatient Management Program Form.
Electroconvulsive Therapy ECT Request Form. Prior Authorization Generic Fax Form PDF 173 KB Prior Authorization Urgent Expedited Fax Form PDF 126 KB Tier Exception PDF 109 KB Prescription drug prior authorization and step therapy exception request forms. Authorization for Disclosure of Mental Health Clinical Information.
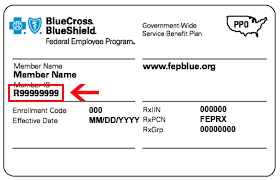
To find a prior authorization form visit our forms page or click on the links below. Supervision via Telehealth Request Attestation. Blue Cross Blue Shield of Mississippi.
Prior authorization sometimes called preauthorization or pre-certification is a pre-service utilization management review. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. Prior authorization is required for some membersservicesdrugs before services are rendered to confirm medical necessity as defined by the members health benefit plan.
Applied Behavior Analysis ABA forms. Once the form is submitted by the physicianmedical office and reviewed by the appropriate pharmacy benefit manager PBM the patient will receive a statement of approval or denial of the requested drug. Behavioral Health for Other BCBSTX Plans.
Health Care Services Referral Form To refer a patient who is a BlueCross BlueShield member to our disease management case management or health coaching service complete and fax this form. BCBSM requires prior authorization for services or procedures that may be experimental not always medically necessary or over utilized. Coordination of Care Form.
NYS Medicaid Prior Authorization Form for Prescriptions. Individual and Family Plans. If you are a Mississippi Network Provider you should submit your Prior Authorization requests through our secure my Blue Provider website.
Blue Advantage Drug Prior Authorization. Medications that Require Prior Authorization M indicates the pre-authorization is only required for Medex and Blue Care 65 members. Prior authorization is required for any inpatient psychiatric care regardless of whether the care is related to autism.
ABA Initial Assessment Request. This request form is used to ensure that the patient in question is receiving the most appropriate and cost-effective treatment available. Submit an Outpatient and Professional Services Authorization Request Submit a Mental Health and Substance Abuse Prior Approval Form Submit a Prescription Drug Prior Authorization Request.
Blue Advantage Physician Drug Authorization Request Form. A prior authorization is not a guarantee of. Applied Behavior Analysis ABA Initial Assessment Request Form.
Electronic Data Interchange EDI Prior Authorization. Carewise audit appeals should go directly to Carewise as noted in the letter sent to providers. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
Prior authorization is required for the initial autism assessment. Behavioral Health Case Management Prescreening. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost.
Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its required. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Requests for the following services can be made by fax or mail.
Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. AUTHORIZATION REQUEST FORM This form is for authorization of prescription drug benefits only and must be COMPLETELY filled out. Form Title Networks Applied Behavior Analysis ABA Clinical Service Request Form.
Member authorization is embedded in the form for providers submitting on a. ABA Clinical Service Request Form. Behavioral Health Substance Abuse Continued Stay Review Form.
Policies Guidelines. Appeal submission with authorization - Resolve billing issues that directly impact payment or a write-off amountNote the different fax numbers for clinical vs. The prior authorization for ABA therapy is.
For ERS or TRS participants refer to specific form links above Form. Prior authorization is also required for ABA therapy. Patient Care Patient Care.
This list shows prescription medications that require your doctor to obtain authorization from us. Submit a prior authorization Reviewed by BlueCross BlueShield. GENERAL INFORMATION Patient Name Request Type please check one Prior Authorization Step Therapy Exception Request for Quantity Limit Exception City Appeal Mandatory Generic Exception Request for Non-Formulary Exception.
Https Webstatic Bcbsms Com Blueland Provider Howtoguides Ecredentialing 12032012 Pdf
Http Webstatic Bcbsms Com Pdf Bcbs 28466 Opioid Medical Policy Non Network Providers Pdf
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
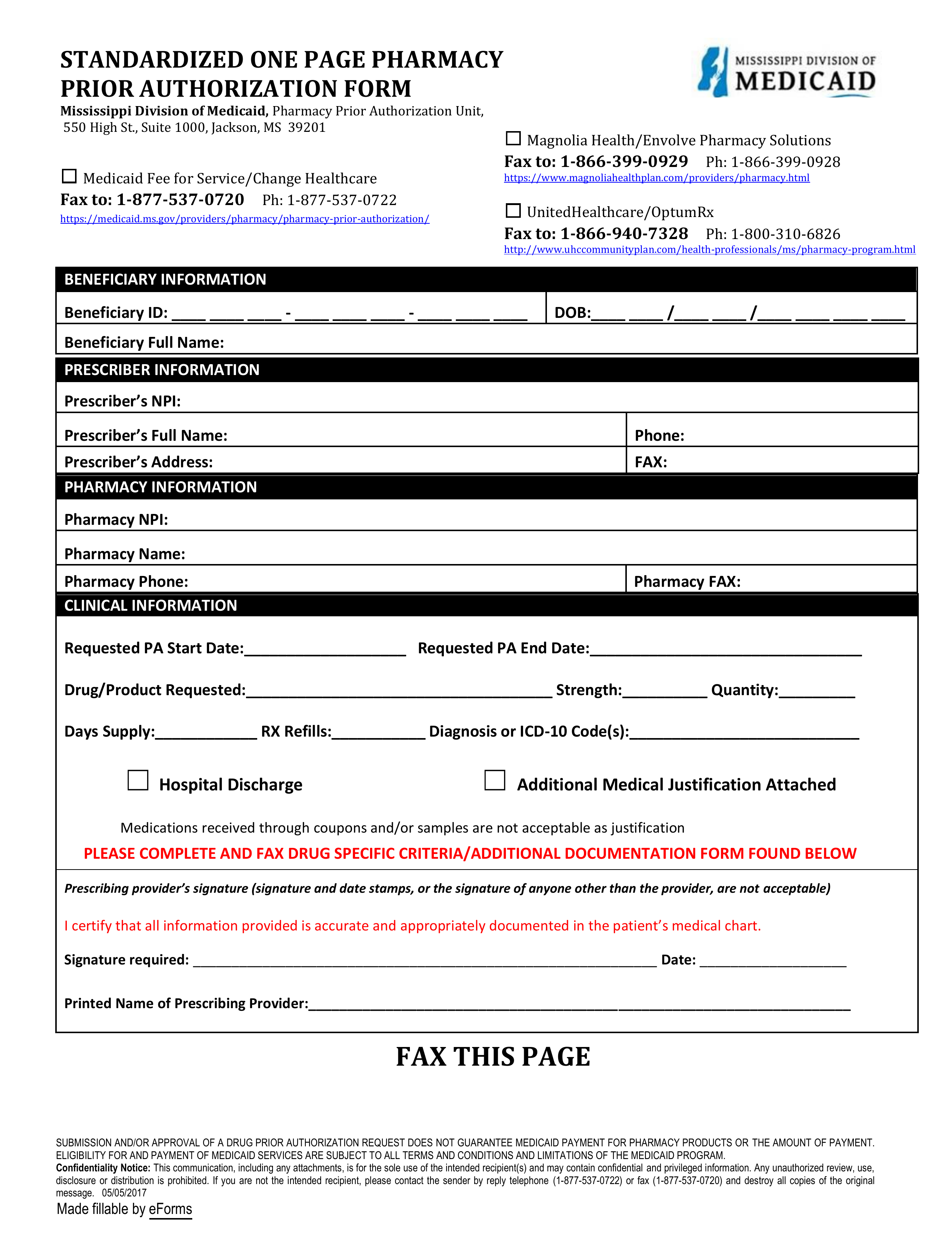
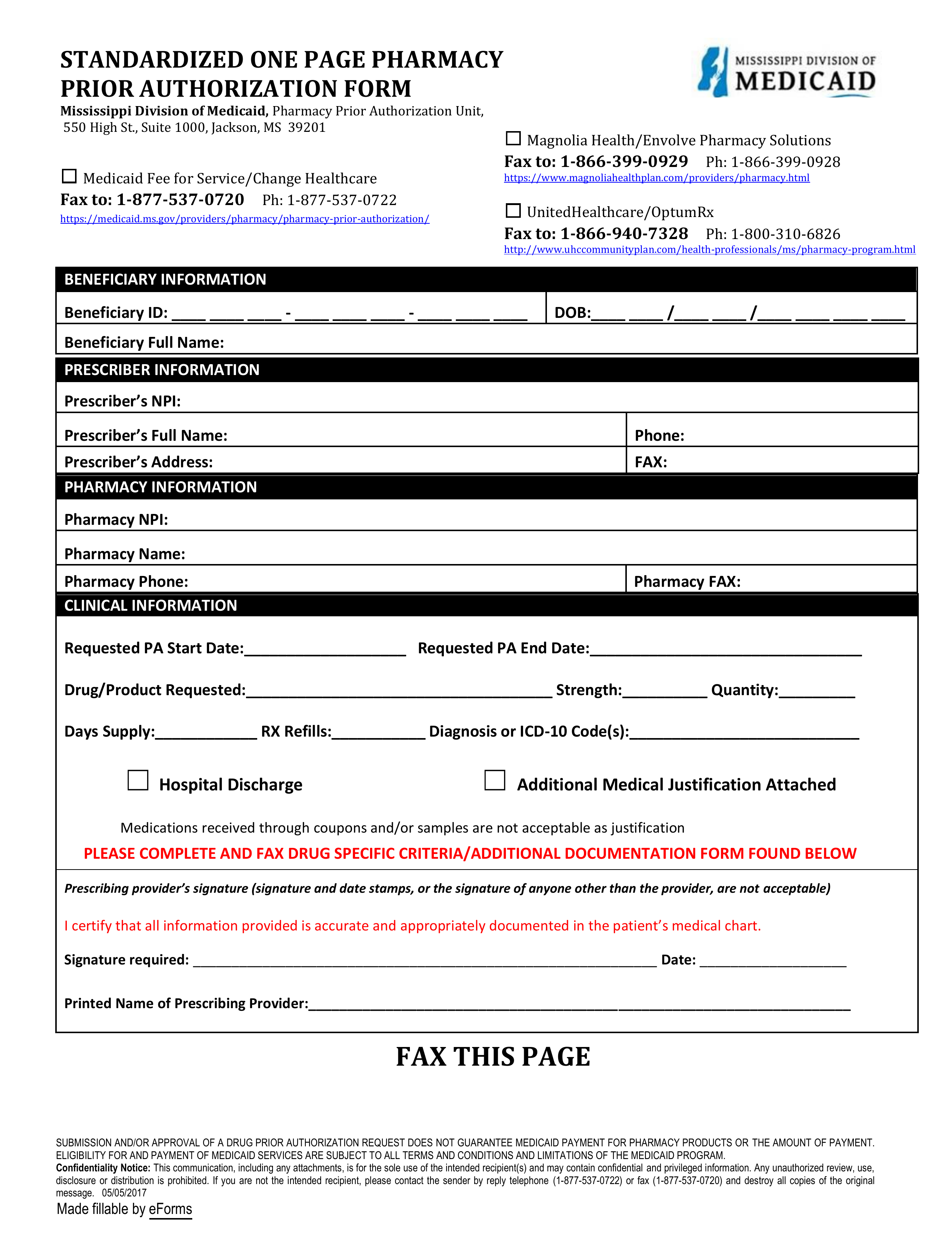 Free Mississippi Medicaid Prior Rx Authorization Form Pdf Eforms
Free Mississippi Medicaid Prior Rx Authorization Form Pdf Eforms
 Blue Advantage Bcbs Medicare Part D Prescription Drug Authorization Request Form 2015 2021 Fill And Sign Printable Template Online Us Legal Forms
Blue Advantage Bcbs Medicare Part D Prescription Drug Authorization Request Form 2015 2021 Fill And Sign Printable Template Online Us Legal Forms
 Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
 Prior Authorization Form Mississippi Medicaid Fill Online Printable Fillable Blank Pdffiller
Prior Authorization Form Mississippi Medicaid Fill Online Printable Fillable Blank Pdffiller
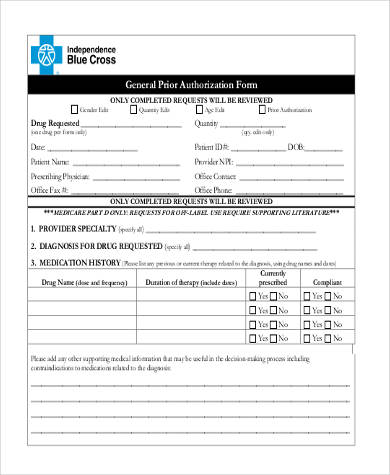 Free 8 Prior Authorization Form Samples In Pdf Ms Word
Free 8 Prior Authorization Form Samples In Pdf Ms Word
 Bcbs 22287 Prior Author Request Blue Cross Blue Shield Of
Bcbs 22287 Prior Author Request Blue Cross Blue Shield Of
 Fillable Online Bcbs Request For Prior Authorization Form Fax Email Print Pdffiller
Fillable Online Bcbs Request For Prior Authorization Form Fax Email Print Pdffiller
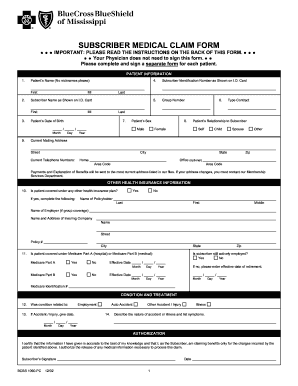
 Ms Bcbs Form Fill Online Printable Fillable Blank Pdffiller
Ms Bcbs Form Fill Online Printable Fillable Blank Pdffiller
 Blue Cross Blue Shield Of Mississippi Prior Authorization Request
Blue Cross Blue Shield Of Mississippi Prior Authorization Request
 Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
B C B S M S P R I O R A U T H O R I Z A T I O N F O R M S P
Comments
Post a Comment