Featured
- Get link
- X
- Other Apps
Medicare Prior Authorization Form Pdf
You may also ask us for a coverage determination by calling the member services number on the back of your ID card. Medicaid Rx Prior Authorization Forms.
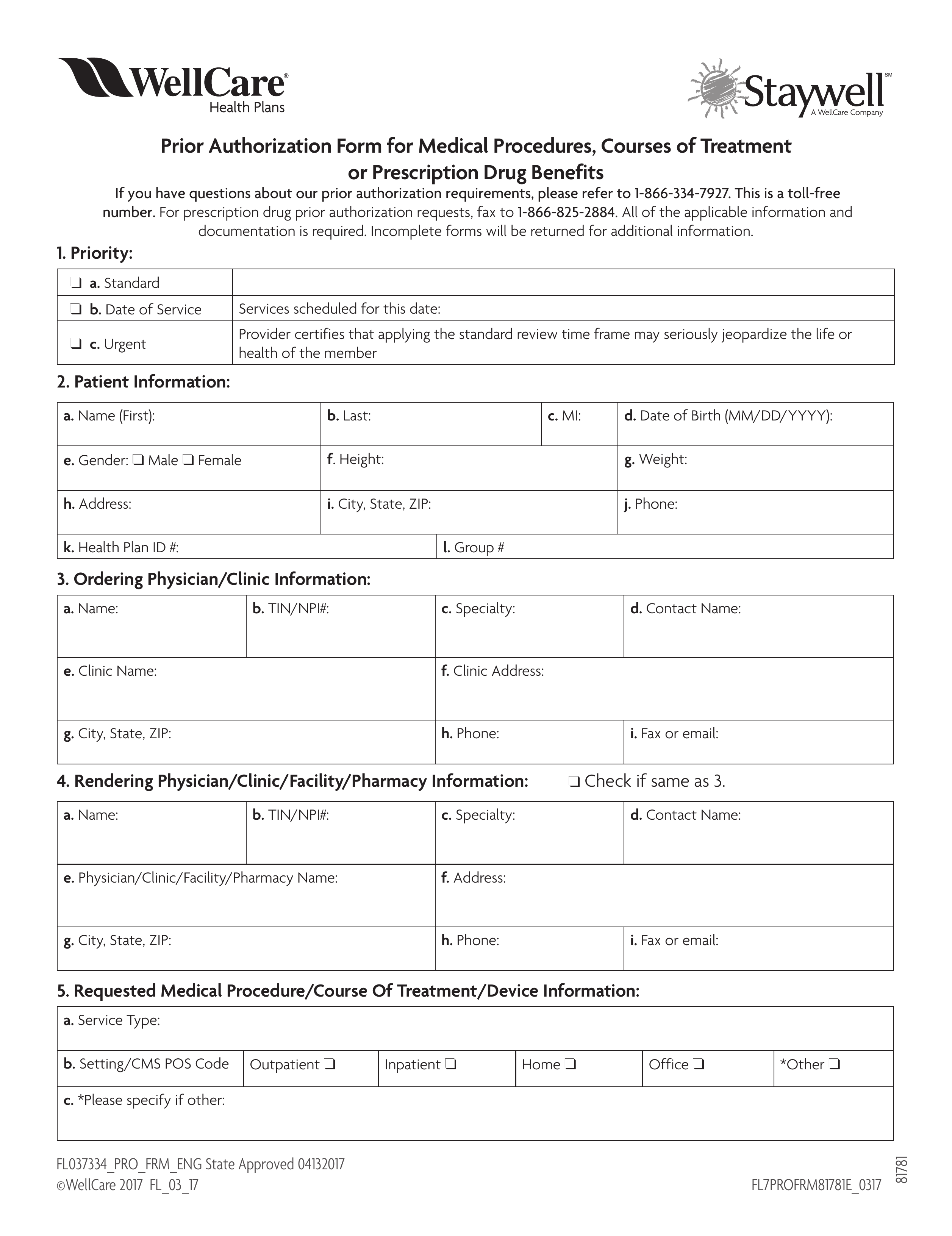 Free Wellcare Prior Rx Authorization Form Pdf Eforms
Free Wellcare Prior Rx Authorization Form Pdf Eforms
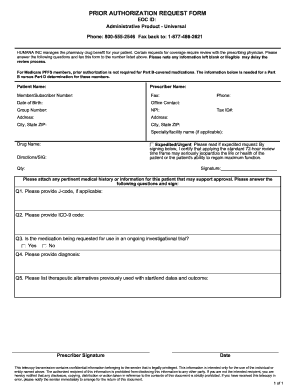
I attest that the medication requested is medically necessary for this patient.
Medicare prior authorization form pdf. Medicare Plus Blue PPO non-Michigan Skilled Nursing Facility Acute Rehabilitation Facility Fax Assessment Form PDF Medicare Plus Blue PPO LTACH Fax Assessment Form PDF Medicare Plus Blue PPO. Enrollment forms I have Part A and want to apply for Part B Application for Enrollment in Part BCMS-40B. Prior authorization helps to ensure that all applicable Medicare coverage payment and coding.
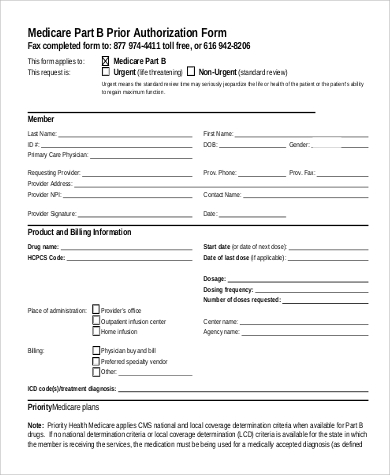
1-844-403-1028 Prior Authorization Department. LTACH and Skilled Nursing Facility Enhancement Assessment Form PDF Blue Cross PPO Request for Preauthorization Form PDF Medicare Plus Blue PPO. Request for Redetermination of Medicare Prescription Drug Denial.
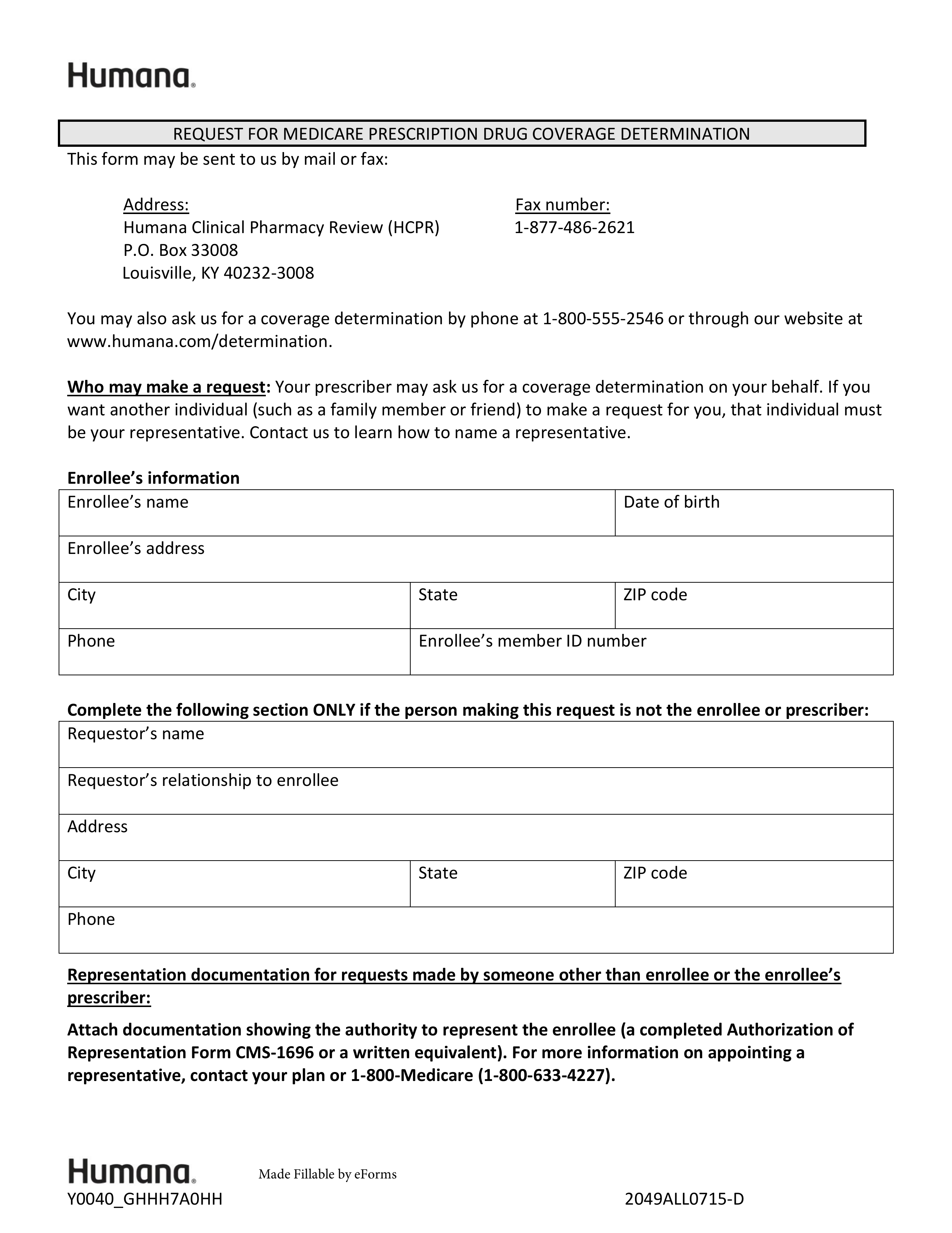
What form do I use to submit a prior authorization request and is it available on the website. Get the SF-5510 as a PDF form in Spanish or HMTL form in Spanish. Request for Medicare Prescription Drug Coverage Determination - Medicare.
Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. Authorized Representative Request PDF Medicare Member Authorization Appeal-appealing Medicare denials of medical prior authorization precertification requests PDF Medicare Non-contracted Provider Appeal Process PDF Medicare Appeals Provider Memo- Post Service PDF. The CVSCaremark prior authorization form is to be used by a medical office when requesting coverage for a CVSCaremark plan members prescription.
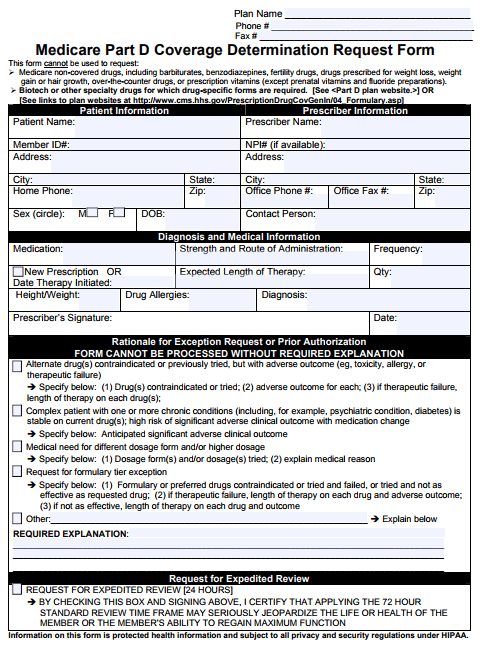
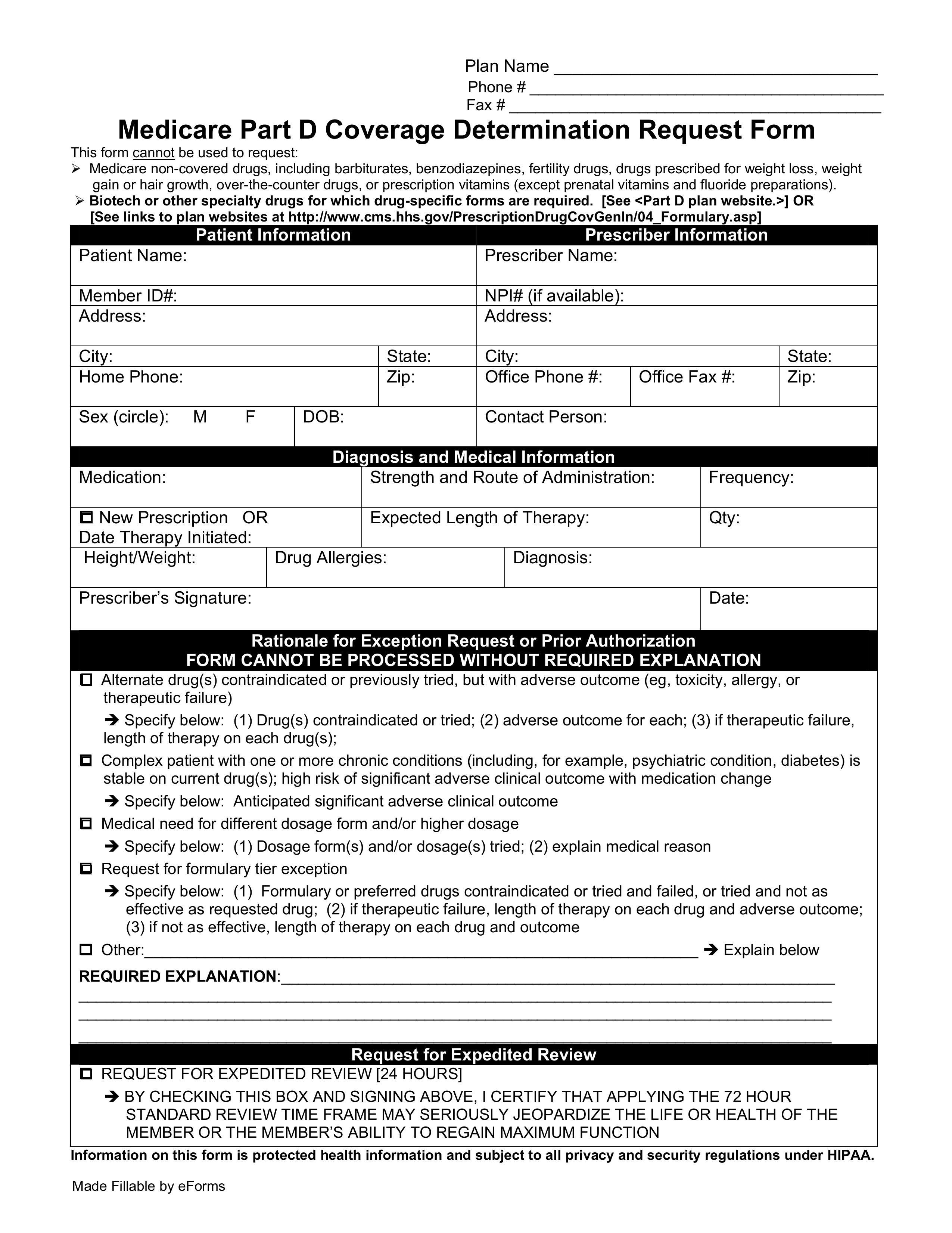
PLEASE FAX COMPLETED FORM TO 1-888-836-0730. REQUEST FOR MEDICARE PRESCRIPTION DRUG COVERAGE DETERMINATION. Step 2 In Patient Information provide the patients full name phone number full address date of birth sex mf height and weight.
Whose prescription drug coverage was sold in the state of California. There is no specific form to request prior authorization. Opens a new window or tab.
The full list of HCPCS codes requiring prior authorization is available here PDF. Fill out the Application for Enrollment in Part B CMS-40B. The Medicaid prior authorization forms appeal to the specific State to see if a drug is approved under their coverage.
UnitedHealthcare Prior Rx Authorization Form. In some cases a physician may choose to prescribe medication that is not on the preferred drug list PDL and will have to fill out a UnitedHealthcare prior authorization form. A physician will need to fill in the form with the patients medical information and submit it to CVSCaremark for assessment.
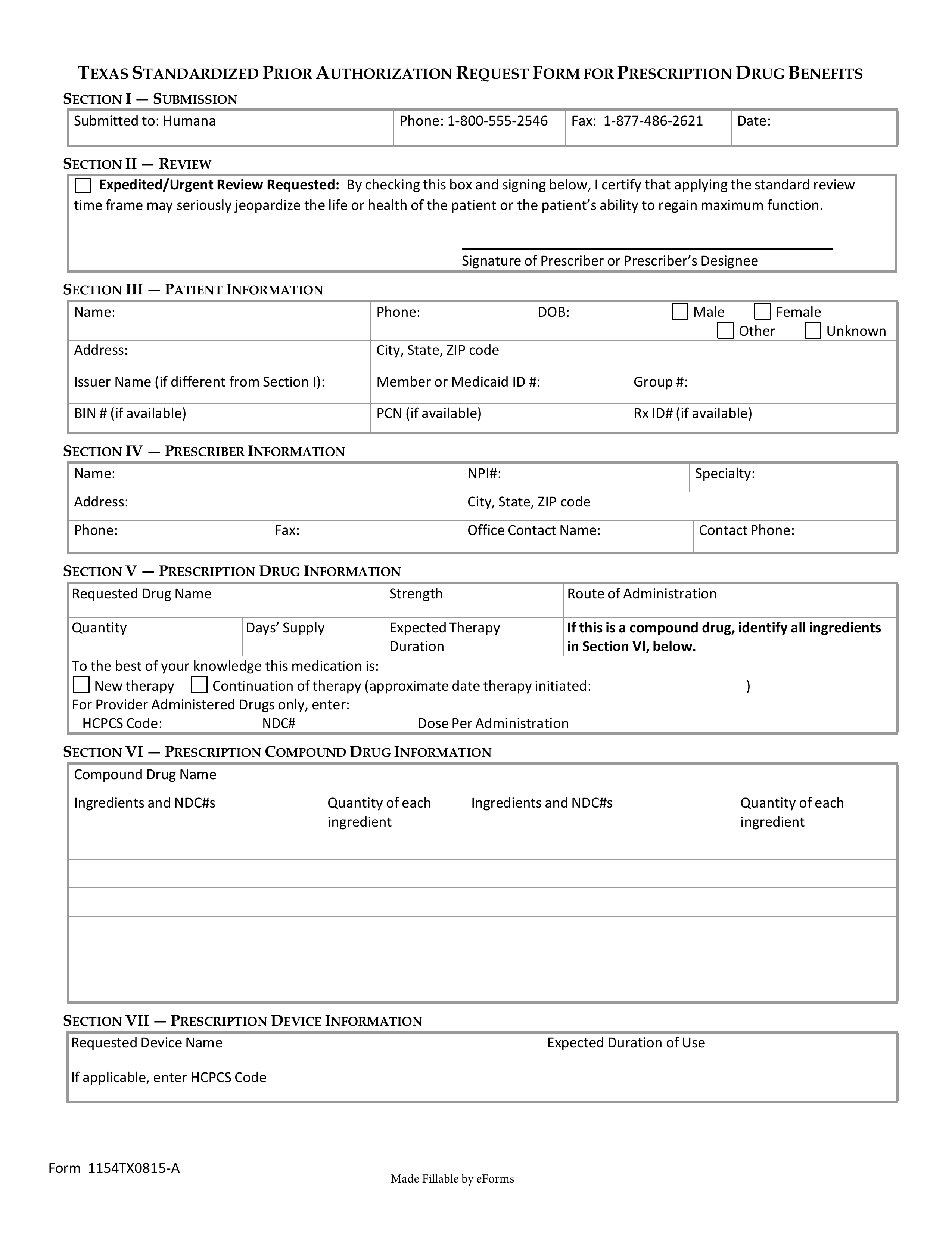
Who reside in the state of California andor. For Part D prior authorization forms please see the Medicare section. The use of this form is mandated for prior authorization requests concerning commercial fully insured members.
Prior authorization is a process through which a request for provisional affirmation of coverage is submitted for review before a service is furnished to a Medicare patient and before a claim is submitted for payment. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Starting February 1 2021 MACs began calculating the affirmation rate of initial prior authorization requests submitted.
This form is to be completed by the patients medical office to see if he or she qualifies under their specific diagnosis and why the drug should be used over another type of medication. Fill out and submit this form to request prior authorization PA for your Medicare prescriptions. Santa Ana CA 92799.
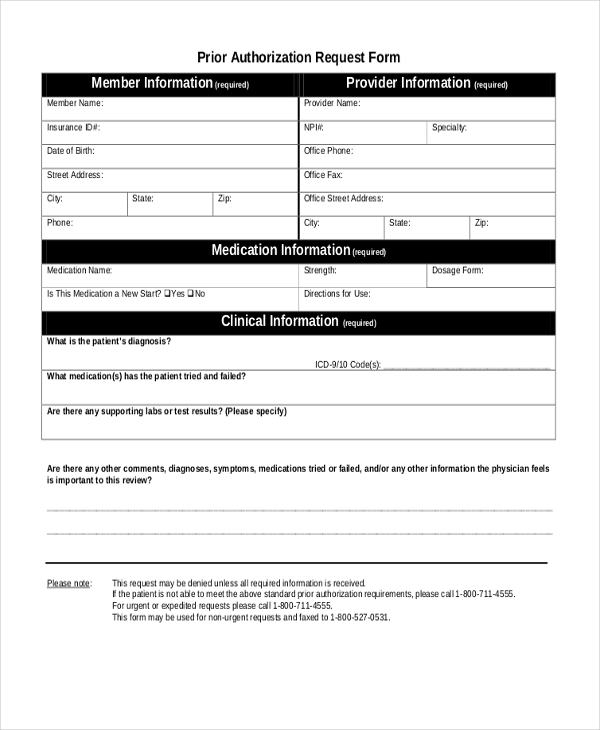
Step 1 At the top of the form supply the planmedical group name planmedical group phone number and planmedical group fax number. I further attest that the information provided is accurate and true and that documentation supporting this. Prior Authorization Request Form Page 1 of 2 DO NOT COPY FOR FUTURE USE.
Please submit your request to the fax number listed on the request form with the fax coversheet. This form may be sent to us by mail or fax. You may also initiate your request by phone by calling the number on the back of the members health plan ID card.
Pre-authorization fax numbers are specific to the type of authorization request. Fill out and submit this form to request an appeal for Medicare medications. Persons covered under a UnitedHealthcare Community Plan UHC have access to a wide range of prescription medication.
State-specific prior authorization request form PDF opens new window. Additionally MACs are in the process of identifying those hospital OPDs that will be exempt from the prior authorization process. Standard Prior Authorization Request Form Please submit your request online using our Prior Authorization and Notification tool on Link.
Fill out the Authorization Agreement for Pre-authorized Payments form SF-5510 as a PDF in English or HTML in English. FORMS ARE UPDATED FREQUENTLY AND MAY BE BARCODED Member Information required Provider Information required Member Name. Your Medicare Administrative Contractor MAC may make a cover sheet or.
Prior Authorization Forms and Policies.
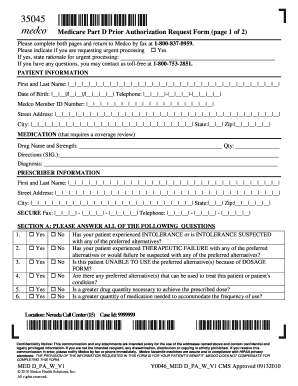 Medco Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Medco Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
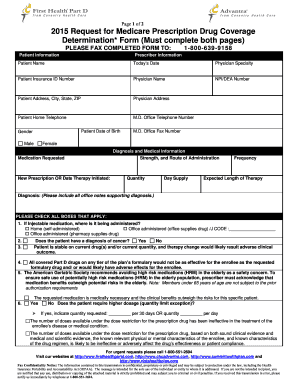 Advantra Silver Prior Auth Form Fill Online Printable Fillable Blank Pdffiller
Advantra Silver Prior Auth Form Fill Online Printable Fillable Blank Pdffiller
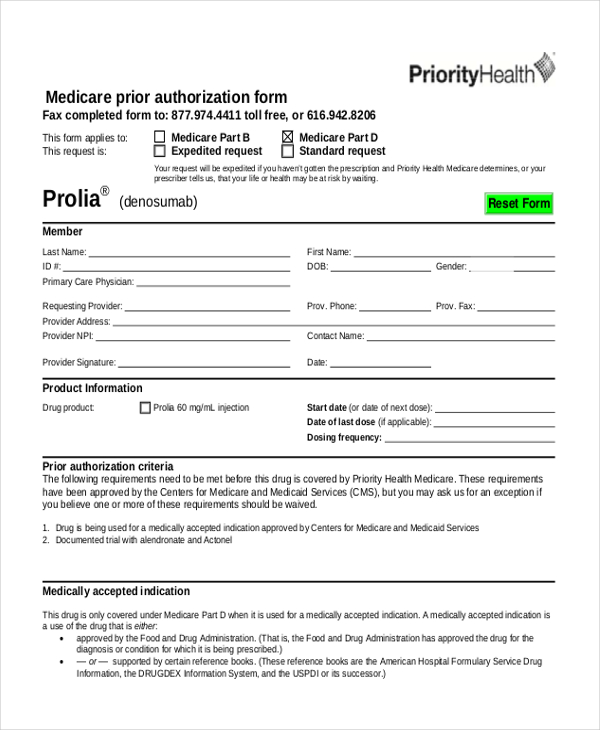
 Priority Health Medical Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Priority Health Medical Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
 Medicare Prior Prescription Rx Authorization Form Authorization Forms
Medicare Prior Prescription Rx Authorization Form Authorization Forms
 Free 9 Sample Prior Authorization Forms In Ms Word Pdf
Free 9 Sample Prior Authorization Forms In Ms Word Pdf
 Free Medicare Prior Rx Authorization Form Pdf Eforms
Free Medicare Prior Rx Authorization Form Pdf Eforms
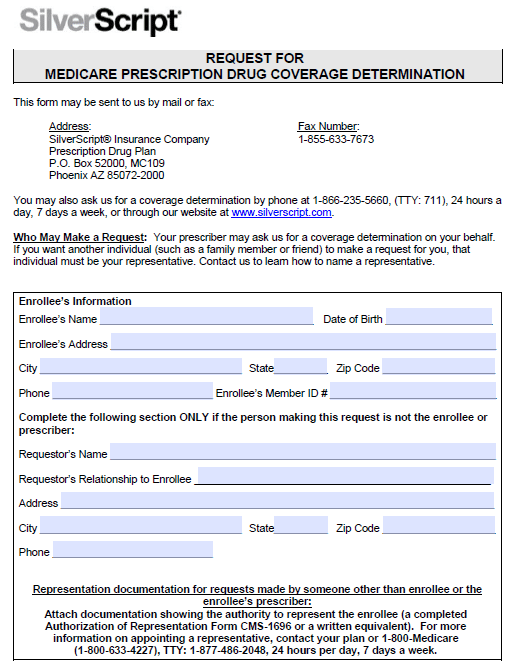 Silverscript Prior Prescription Rx Authorization Form Authorization Forms
Silverscript Prior Prescription Rx Authorization Form Authorization Forms
 Free 10 Sample Medicare Forms In Pdf Ms Word
Free 10 Sample Medicare Forms In Pdf Ms Word
 Free 8 Sample Prior Authorization Forms In Pdf Ms Word
Free 8 Sample Prior Authorization Forms In Pdf Ms Word
Https Www Bcbsm Com Content Dam Public Providers Documents Global Medication Authorization Request Form Pdf
 Free Humana Prior Rx Authorization Form Pdf Eforms
Free Humana Prior Rx Authorization Form Pdf Eforms
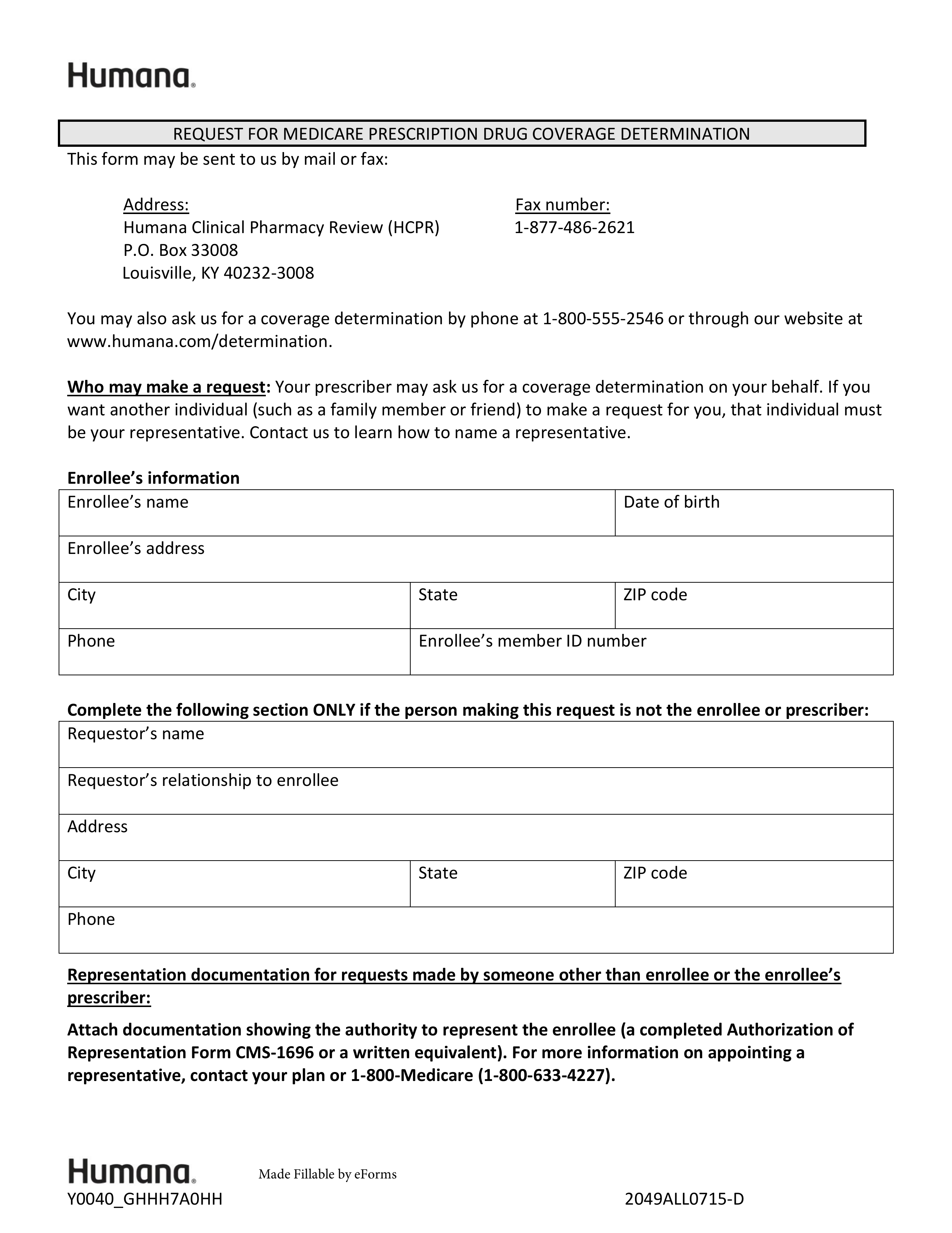 Free Humana Prior Rx Authorization Form Pdf Eforms
Free Humana Prior Rx Authorization Form Pdf Eforms
 Humana Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Humana Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
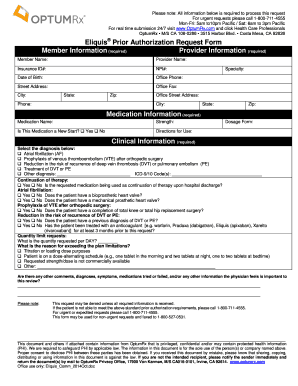 Optumrx Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Optumrx Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Comments
Post a Comment