Featured
- Get link
- X
- Other Apps
Highmark Blue Cross Blue Shield Medication Prior Authorization Forms
Dupixent Prior Authorization Form. CoverMyMeds is Highmark Blue Shield Prior Authorization Formss Preferred Method for Receiving ePA Requests.
 Drug Request Form Fill Online Printable Fillable Blank Pdffiller
Drug Request Form Fill Online Printable Fillable Blank Pdffiller
Chronic Inflammatory Diseases Medication Request Form.
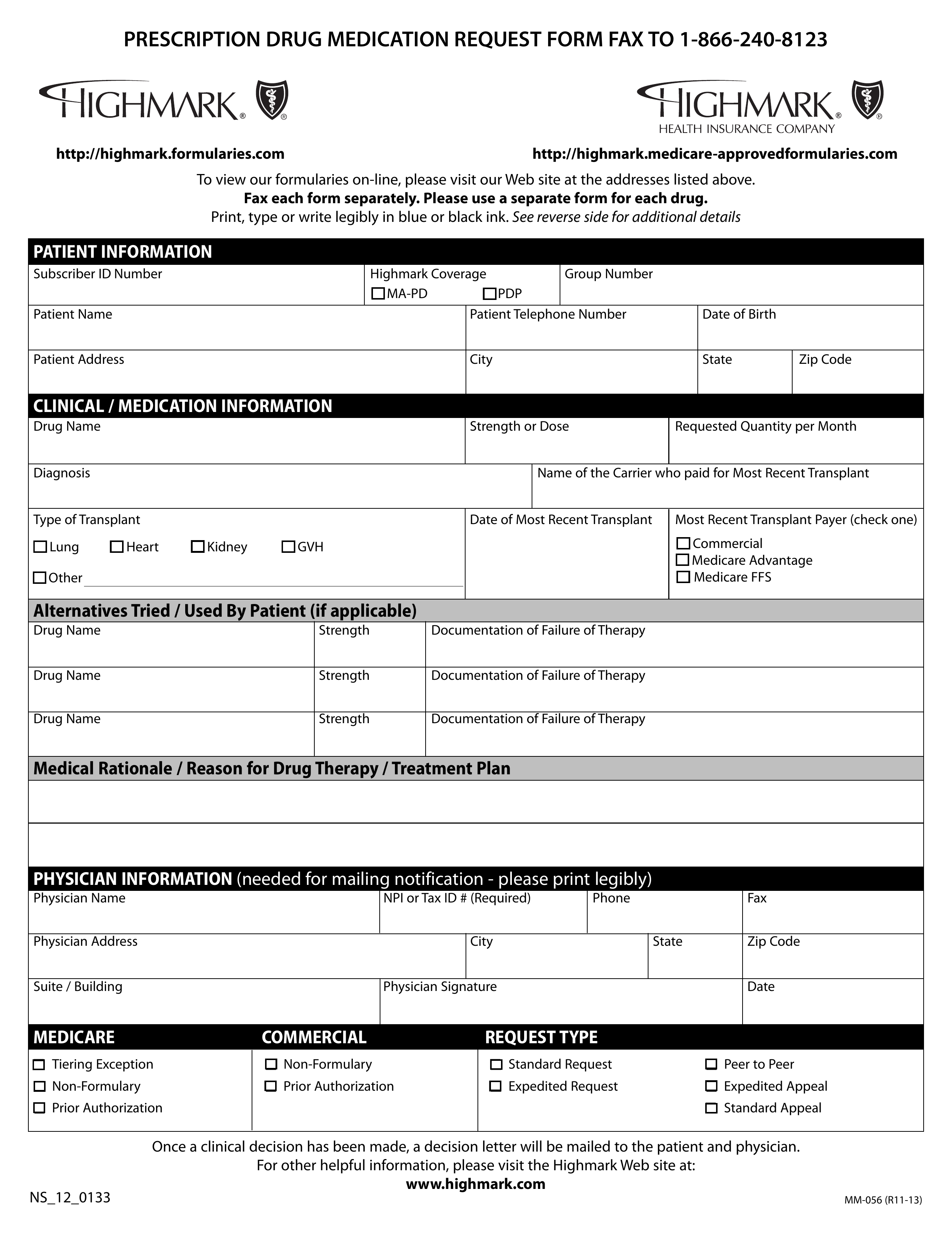
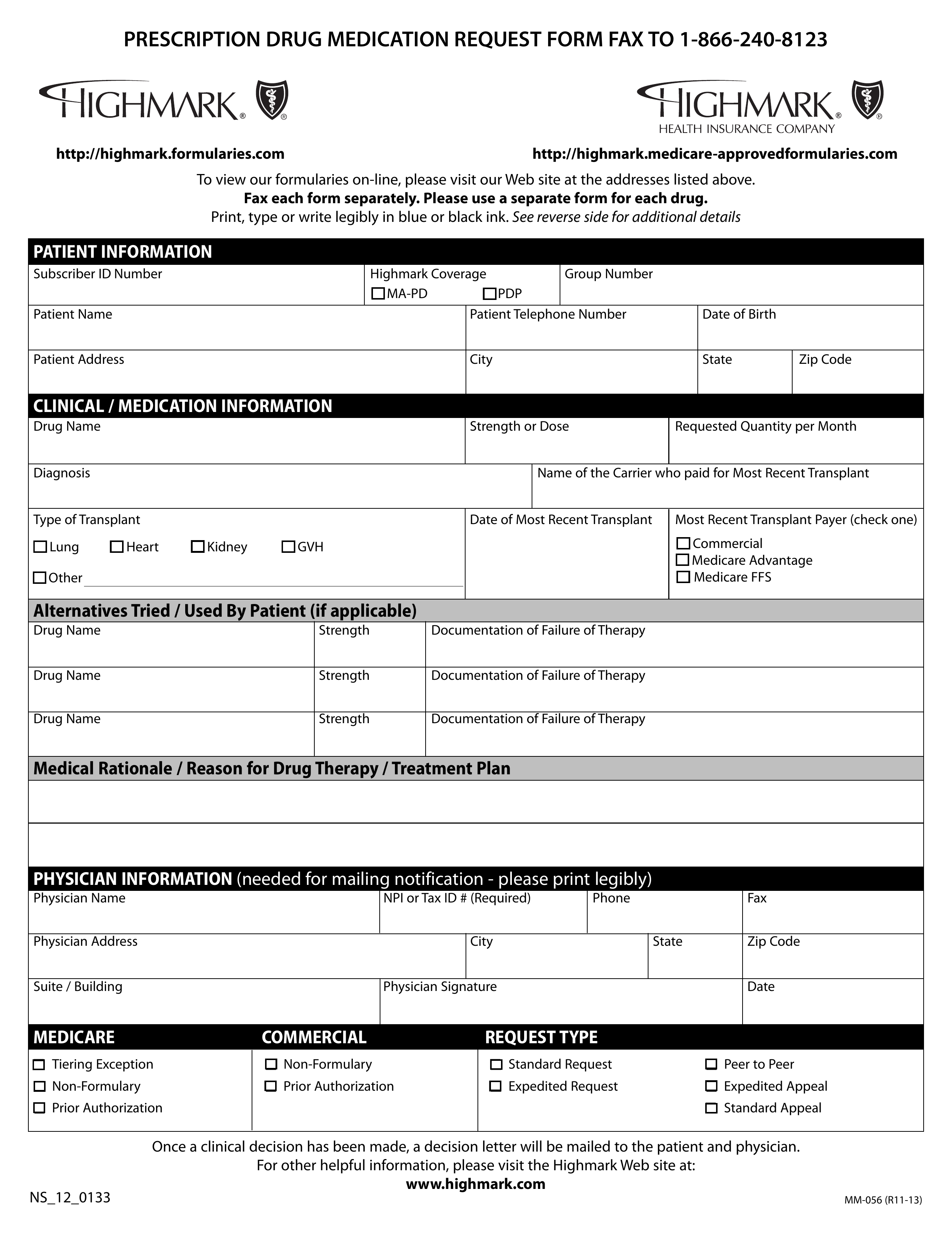
Highmark blue cross blue shield medication prior authorization forms. Submit a separate form for each medication. Please fax the completed form to 716-887-8886. Please note that the drugs and therapeutic categories managed under our Prior Authorization and Managed Prescription Drug Coverage MRXC programs are subject to change based on the FDA approval of new drugs.
Print type or write legibly in blue or. Some authorization requirements vary by. Please provide the physician address as it is required for physician notification.
Fax the completed form to 1-412-544-7546 Or mail the form to. The prescribing physician PCP or Specialist should in most cases complete the form. PCSK9 Inhibitor Prior Authorization Form.
The prescribing physician PCP or Specialist should in most cases complete the form. Some drugs require authorization before they will be covered by the pharmacy benefit program at the point of sale. The prescribing physician PCP or Specialist should in most cases complete the form.
Physicians must use the program to obtain these drugs for their Medicare Advantage FreedomBlueSM patients. Fax the completed form to 1-412-544-7546 Or mail the form to. Highmark members may have prescription drug benefits that require prior authorization for selected drugs.
Professional address changes should be completed by using the. Ad We Accept Orders From GPs The NHS Private Companies And Members Of The Public. Complete ALL information on the form.
Medical Management Policy 120 Fifth Avenue MC P4207 Pittsburgh PA 15222 CLINICAL MANAGEMENT PROCEDURES Drugs that are managed using a Prior Authorization or Managed Prescription Drug Coverage MRXC require the submission of specific medical information prior to authorizing the drug. Ad We Accept Orders From GPs The NHS Private Companies And Members Of The Public. Submit a separate form for each medication.
The Highmark prior authorization form is a document which is used to determine weather or not a patients prescription cost will be covered by their Highmark health insurance plan. Next Day Delivery Available On All Orders Before 6pm. Request to Resolve Provider Negative Balance.
CoverMyMeds automates the prior authorization PA process making it the fastest and easiest way to review complete and track PA requests. Fax each form separately. Medical Pharmacy Affairs PO.
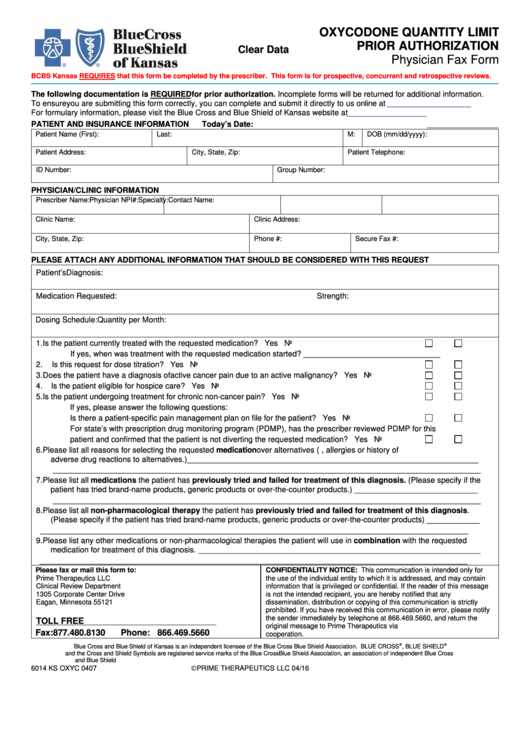
Fax the completed form to 1-866-240-8123 Or mail the form to. Extended Release Opioid Prior Authorization Form. Complete ALL information on the form.
Call the Provider Service Center at 1-866-731-8080 for information regarding specific plans. Medical Pharmacy Affairs. Please use a separate form for each drug.
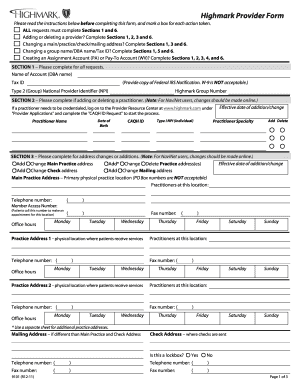
N Prior Authorization n Standard Appeal CLINICAL MEDICATION INFORMATION PRESCRIPTION DRUG MEDICATION REQUEST FORM FAX TO 1-866-240-8123 To view our formularies on-line please visit our Web site at the addresses listed above. Provider Demographic Change Form Please submit this form to our Corporate Provider File Department when adding additional office locations to your practice or if your practice moves from its current location. Highmark Blue Shield has a streamlined program through which all PremierBlue SM Shield network physicians must obtain certain medical injectable drugs.
Fax each form separately. Fax the completed form and all clinical documentation to 888-236-6321 Or mail the completed form to. Print type or write legibly in blue or.
Please provide the physician address as it is required for physician notification. A physician must fill in the form with the patients member information as well as all medical details related to the requested prescription. Once the form is complete send it by fax or mail to the.
AddressPhone Number Change Form for Facility Ancillary Providers. We are committed to providing outstanding services to our applicants and members. Complete ALL information on the form.
N Prior Authorization n Standard Appeal CLINICAL MEDICATION INFORMATION PRESCRIPTION DRUG MEDICATION REQUEST FORM FAX TO 1-866-240-8123 To view our formularies on-line please visit our Web site at the addresses listed above. Please provide the physician address as it is required for physician notification. Modafinil and Armodafinil PA Form.
Complete ALL information on the form. The authorization is typically obtained by the ordering provider. Submit a separate form for each medication.
On this page you will find some recommended forms that providers may use when communicating with Highmark its members or other providers in the network. Information on this website is issued by Highmark Blue Cross Blue Shield on behalf of these companies which serve the 29 counties of western Pennsylvania and 13 counties in northeast and north central Pennsylvania. NOTEThe prescribing physician PCP or Specialist shouldin most casescomplete the form.
Please provide the physician address as it is required for physician notification. Medicare Part D Hospice Prior Authorization Information. Highmark Blue Shield and Highmark Health Insurance Company are independent licensees of the Blue Cross and Blue Shield Association.
Next Day Delivery Available On All Orders Before 6pm. Please use a separate form for each drug. Fax the COMPLETED form to 1-866-240-8123 Or mail to.
The program is optional for PPOBlue SM DirectBlue. This form is to be used for facilityancillary changes. Request for Non-Formulary Drug Coverage.
Medical Injectable Drug Program. Authorization Requirements Highmark requires authorization of certain services procedures andor DMEPOS prior to performing the procedure or service.
Https Www Ibx Com Documents 35221 56677 Prior Auth Botulinum Toxins Pdf 99b5b638 Fc7c 290b Ab03 58c7a997ef40 T 1580924446000
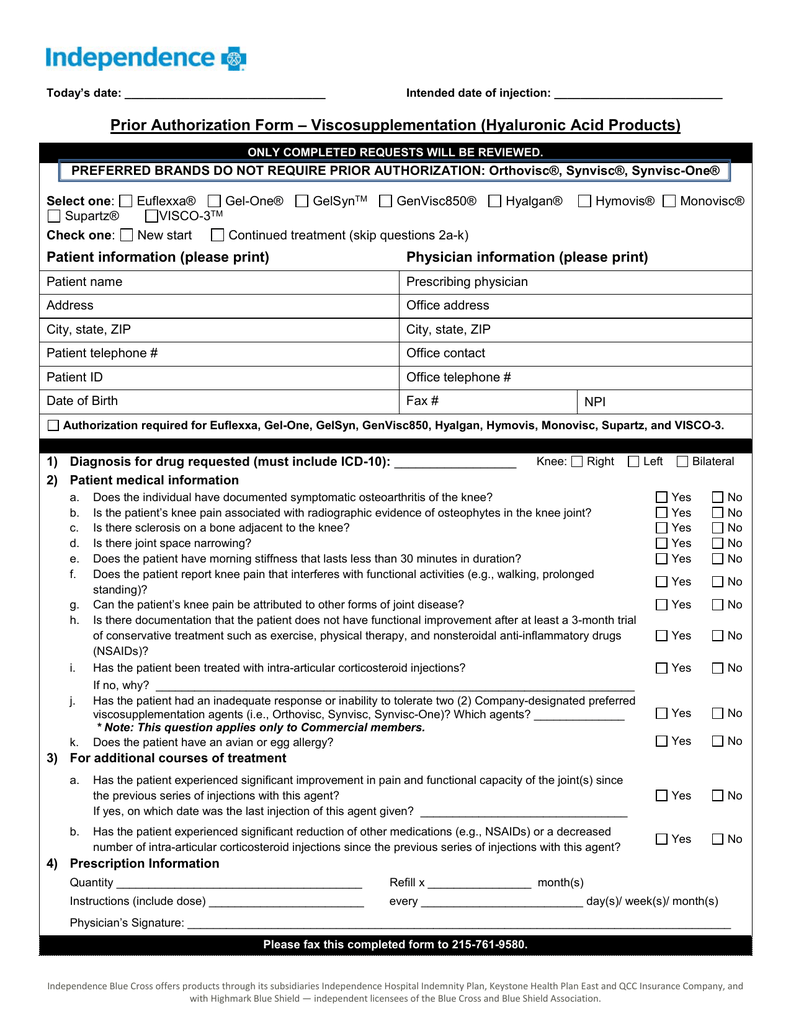 Prior Authorization Form Viscosupplementation Hyaluronic Acid
Prior Authorization Form Viscosupplementation Hyaluronic Acid
 Fillable Online Blue Cross Blue Shield Wv Form Fax Email Print Pdffiller
Fillable Online Blue Cross Blue Shield Wv Form Fax Email Print Pdffiller
 Highmark Bcbs Medication Prior Authorization Form Inspirational Free Resume Format Blue Cross Blue Shield Medication Prior Models Form Ideas
Highmark Bcbs Medication Prior Authorization Form Inspirational Free Resume Format Blue Cross Blue Shield Medication Prior Models Form Ideas
Https Www Ibx Com Documents 35221 56677 Prior Auth Makena Pdf 08bf7ea6 Baa2 Bf95 0587 20c06ca3398f T 1580924446433
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
 Highmark Bcbs Medication Prior Authorization Form Best Of Anthem Express Scripts Prior Authorization Form New Free Gov Forms Models Form Ideas
Highmark Bcbs Medication Prior Authorization Form Best Of Anthem Express Scripts Prior Authorization Form New Free Gov Forms Models Form Ideas
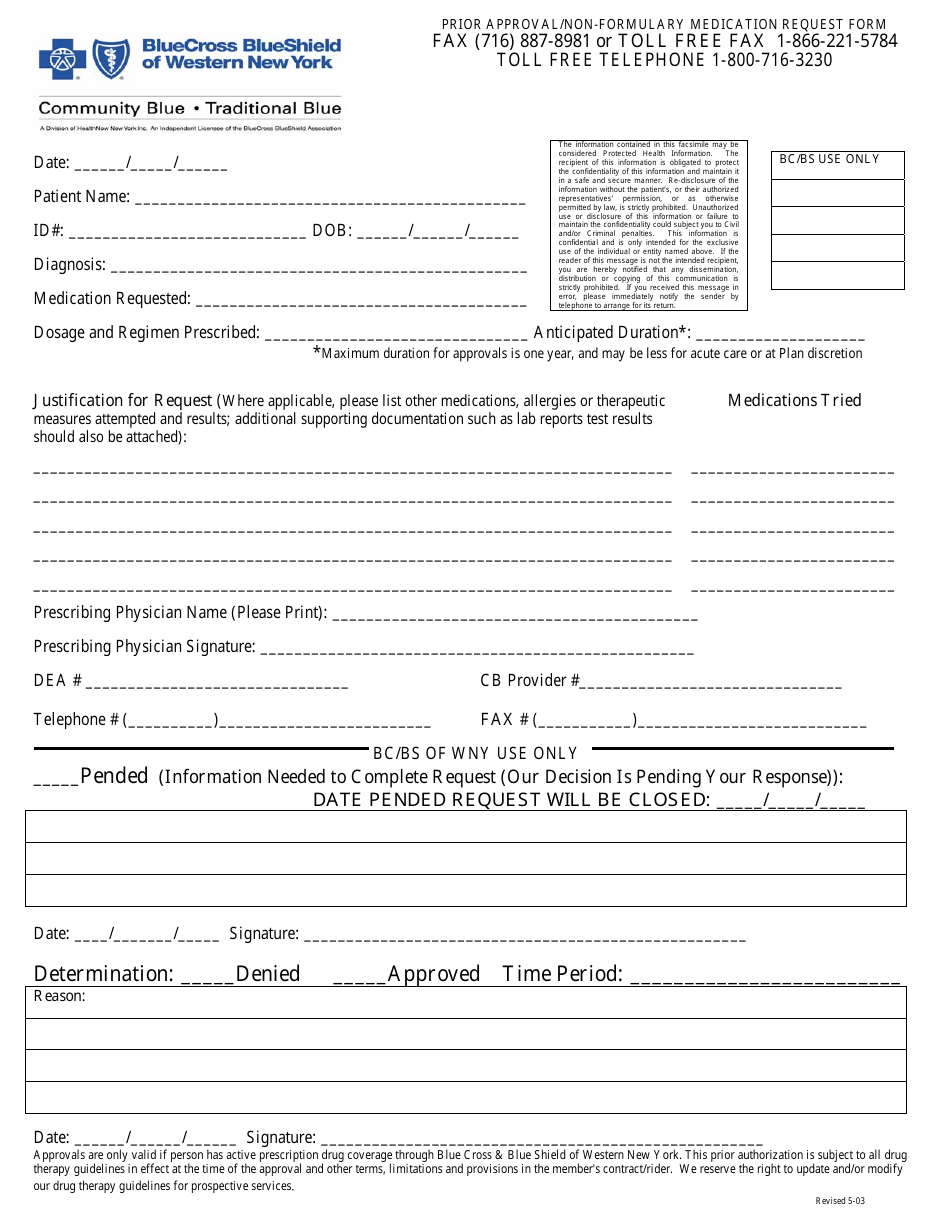 New York Prior Approval Non Formulary Medication Request Form Blue Cross Blue Shield Of Western New York Download Printable Pdf Templateroller
New York Prior Approval Non Formulary Medication Request Form Blue Cross Blue Shield Of Western New York Download Printable Pdf Templateroller
 Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
 H I G H M A R K B C B S P R I O R A U T H O R I Z A T I O N F O R M Zonealarm Results
H I G H M A R K B C B S P R I O R A U T H O R I Z A T I O N F O R M Zonealarm Results
 Free Highmark Prior Rx Authorization Form Pdf Eforms
Free Highmark Prior Rx Authorization Form Pdf Eforms
 Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
Https Www Ibx Com Documents 35221 56677 Prior Auth Prolia Xgeva Pdf 77e8577f Ec58 32b6 67a2 0b4eff40815c T 1580924446700
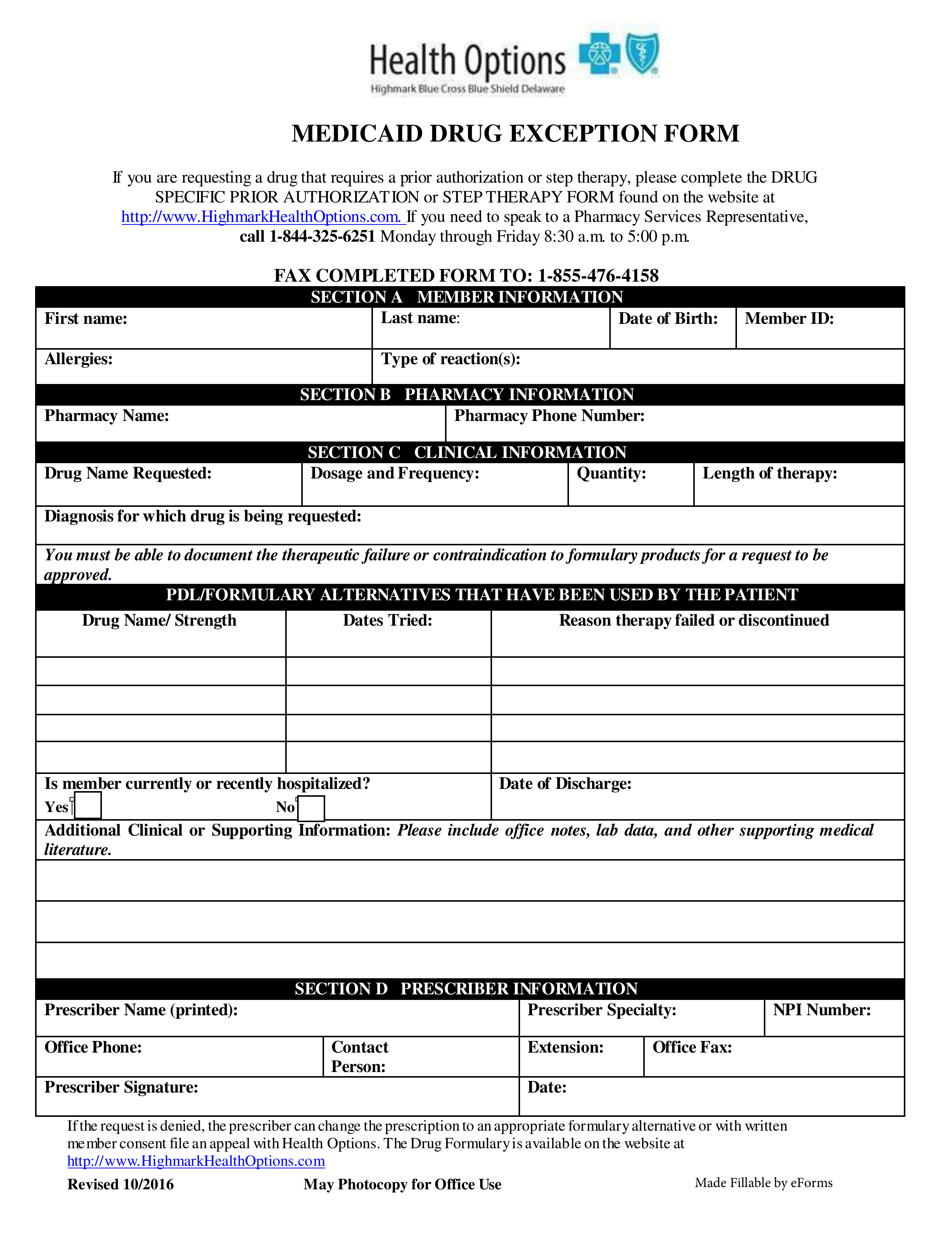 Free Delaware Medicaid Prior Rx Authorization Form Pdf Eforms
Free Delaware Medicaid Prior Rx Authorization Form Pdf Eforms
Comments
Post a Comment