Featured
- Get link
- X
- Other Apps
Anthem Medicare Advantage Prior Authorization
You will be directed to the Medicare Advantage. Southern Company offers Medicare Advantage option.
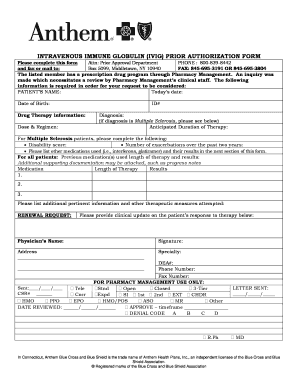 Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
New Hampshire Medicare Advantage Plans include all the benefits of Original Medicare Parts A and B plus extra benefits for Medicare-eligibles like vision and dental insurance and hearing coverage.

Anthem medicare advantage prior authorization. Jul 1 2020 State Federal Medicare. This will help prevent the need for additional outreach to Anthem to adjust the date of service covered by the authorization. Effective January 1 2021 Southern Company retirees who are eligible for Medicare Parts A and B will be enrolled in an Anthem Medicare Preferred PPO plan.
Federal and state law as well as state contract language and Centers for Medicare Medicaid Services guidelines including definitions and specific contract provisionsexclusions. Anthem Blue Cross and Blue Shield is a DSNP plan with a Medicare contract and a contract with the state Medicaid program. If you choose to see a provider outside your plan your costs may be higher.
Dec 1 2020 State Federal Medicare. A Medicare Advantage PPO plan is a Part C plan that works like a Preferred Provider Organization PPO plan. Advantage members also will have new utilization management and prior authorization requirements.
Medicare Advantage Plans Part C These all-in-one plans combine Part A B and D to give you more than just Original Medicare. Most of our Medicare Advantage plans include coverage for prescription drugs dental vision and hearing aids. The Anthem Medicare Preferred PPO plan will replace the current Southern Company post-65.
AIM Specialty Health AIM currently performs utilization management review for bilevel positive airway pressure BiPAP equipment and all associated supplies. We are currently in the process of enhancing this forms library. Medicare Advantage Providers Anthem offers a variety of Medicare plans to support member needs.
2018 Medicare Advantage individual benefits and formularies 41 2018 Annual visit guidelines 41 Anthem tiers SNF network 41 Change to the 835 Electronic Remittance Advice for all MA members enrolled in D-SNPs 42 Dual eligible special needs plans provider training required 42 Anthem to conduct post -payment reviews of certain modifiers. Attention Prescribing Providers with members who are enrolled in an Anthem California planThe Prescription Drug Prior Authorization Or Step Therapy. Contracted and Non-contracted providers should contact the Health Plan if they are not able to access Availity.
Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. They also offer benefits such as SilverSneakers fitness memberships money for over-the-counter items and.
Go to Auths and ReferralsAuthorizations from the left navigation menu. During this time you can still find all forms and guides on our legacy site. Easily find and download forms guides and other related documentation that you need to do business with Anthem all in one convenient location.
Plus these plans often have extras such as coverage for prescription drugs vision dental and hearing aids. Prior authorization codes moving from AIM Specialty Health to Anthem Blue Cross and Blue Shield. Provider Forms Guides.
Select Anthem Medicare Advantage from the drop down box. For costs and complete details of the coverage please contact your agent or the health plan. Please see the Group Medicare Drug Listspage or call Customer Service at the number on the back of your membership card for information on requirements which apply to the Group Medicare Prescription plans.
These services utilization management and prior authorization requirements already are in place for many Anthem individual Medicare Advantage. Contracted and non-contracted providers who are unable to access Availity may call the number on the back of the members ID card. Anthem MediBlue HMO Medicare Advantage plans bundle all the benefits of Medicare Part A and Medicare Part B into one convenient plan.
Extending the length of time a prior authorization issued on or before May 30 2020 is in effect for elective inpatient and outpatient procedures to 180 days. Anthem MediBlue PPO is a Medicare Advantage plan that gives you the flexibility to work with any doctor or specialist in or out of network no referrals needed. Medicare Advantage Plans requiring in-network provider precertification.
Although prior authorization is not required Anthem requests voluntary notification via the usual channels to aid in our members care coordination and management. The bill seeks to streamline the prior authorization process in Medicare Advantage by requiring insurers adopt electronic programs provide real-time determinations for some services and release. We also support our providers with access to information about our plans and member benefits news and updates training materials and guides and other helpful resources.
Medicare Advantage members with alpha prefixes YGZ MHG MBL and ZDX are group-sponsored Medicare Advantage members who are eligible for the services and the utilization management and prior authorization requirements listed below. Medicare Part C is also called Medicare Advantage MA. Youll have no copays for preventive care like your yearly check-ups and get 0 copays for dental and vision.
Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Anthem Blue Cross and Blue Shield is a Medicare Advantage plan with a Medicare contract. Detailed Prior Authorization requirements are available to the contracted provider by accessing the Provider Self-Service Tool within Availity.
Effective June 1 2020 prior authorization PA requirements will change for the following services to be covered for Anthem Blue Cross members. Beginning July 1 2020 the following codes will require prior authorization with Anthem.
Https Www Anthem Com Provider Noapplication F4 S6 T0 Pw E213404 Pdf Refer Ahpprovider State Ct
Https Www Anthem Com Ca Shared F2 S2 T1 Pw G345985 Pdf Refer Culdesac Name Ssb
 Collection Blue Cross Blue Shield Prior Authorization Form Models Form Ideas
Collection Blue Cross Blue Shield Prior Authorization Form Models Form Ideas
Https Mss Anthem Com California Mmp Caca Mmp 2020coveragedeterminationform Eng Pdf
 A N T H E M M E D I C A R E P R I O R A U T H O R I Z A T I O N F O R M Zonealarm Results
A N T H E M M E D I C A R E P R I O R A U T H O R I Z A T I O N F O R M Zonealarm Results
 A N T H E M P R I O R A U T H O R I Z A T I O N F O R M Zonealarm Results
A N T H E M P R I O R A U T H O R I Z A T I O N F O R M Zonealarm Results
Https Www Anthem Com Ca Shared F2 S2 T1 Pw E245496 Pdf Refer Provider
Https Www11 Anthem Com Ca Shared F2 S2 T1 Pw G337152 Pdf Refer Provider
 Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Https Www11 Anthem Com Ca Shared F2 S2 T1 Pw E245586 Pdf Refer Provider
Https Www11 Anthem Com Ca Shared F2 S2 T1 Pw G381575 Pdf Refer Provider
 Anthem Healthkeepers Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Healthkeepers Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
 Anthem Healthkeepers Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Healthkeepers Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Comments
Post a Comment