Featured
- Get link
- X
- Other Apps
Tricare West Prior Authorization
Tricares Preferred Method for Prior Authorization Requests CoverMyMeds is the fastest and easiest way to review complete and track PA requests. First make sure your service requires authorization by checking HNFS Prior Authorization and Referral Benefit tool.
 Tricare Medication Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Tricare Medication Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
For all other plans.
Tricare west prior authorization. Medicare-eligible beneficiaries do not need prior authorization for behavioral health admissions when Medicare is the primary payer. Requesting Prior Authorization If youre enrolled in a TRICARE Prime plan your primary care manager PCM will work with your regional contractor for the prior authorization. It is our privilege to work alongside VA as we provide Veterans with access to high.
Getting prior authorization means youre getting the care approved by your regional contractor before you actually go to an appointment and get the care. Use the Prior Authorization Referral and Benefit Tool to find out if a service requires a Health Net referral or prior authorization. Comply with our simple steps to get your Tricare West Region EFT Authorization Request well prepared rapidly.
Be sure an authorization is in place so you dont have to pay for the services out. View a tutorial for a step-by-step process of entering a new request andor checkupdate an existing referral or authorization. If youre not required to get referrals you should know what services need prior authorization.
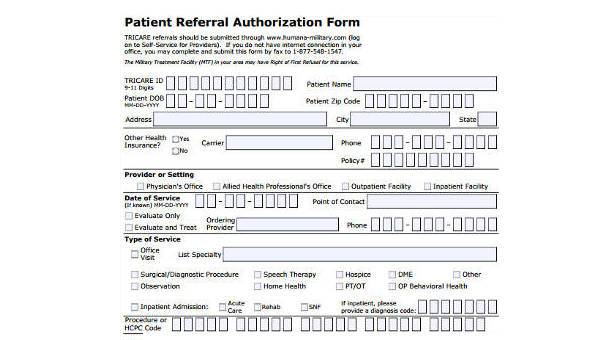
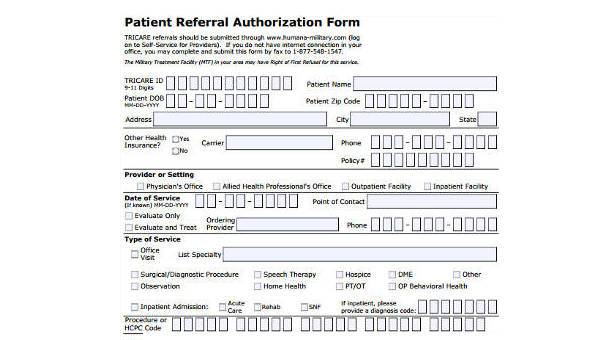
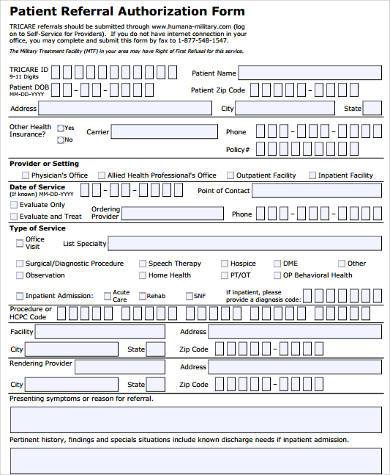
Our electronic prior authorization ePA solution is HIPAA-compliant and available for all plans. When completing the referral always include the sponsors TRICARE ID diagnosis and clinical data explaining the reason for the referral. Have you checked requirements.
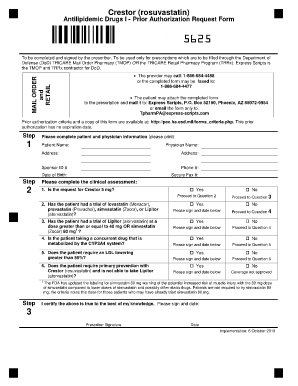
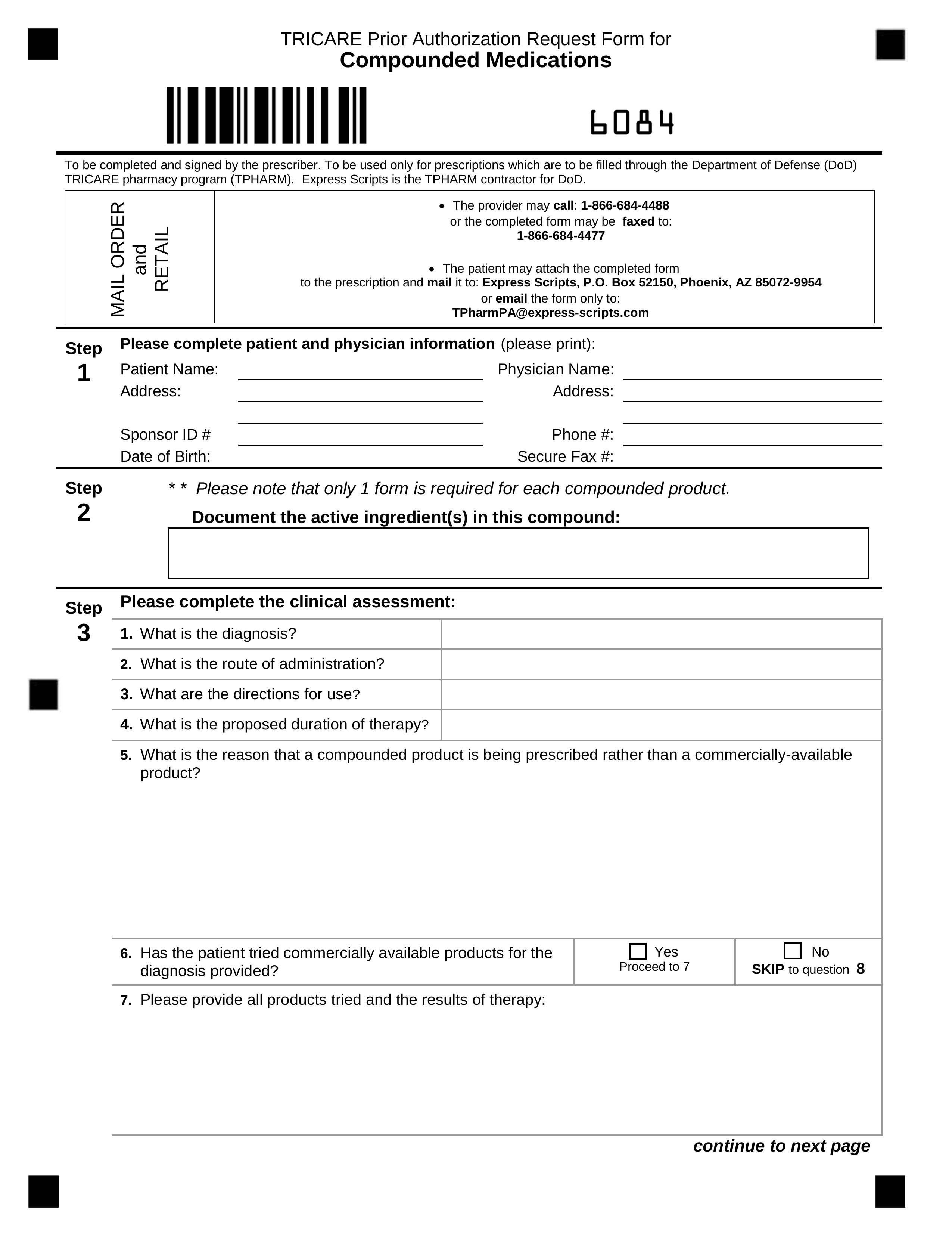
The user-friendly dragdrop graphical user interface allows you to include or relocate areas. Select the template from the library. How to Get Prior Authorization Search for your drug on the TRICARE Formulary Search Tool Download and print the form for your drug.
If Medicare or another primary insurance covers the care then no authorization review is necessary. A TRICARE prior authorization form is a document to be completed by a prescribing physician requesting a specific type of medication for their patient which is otherwise not covered by their TRICARE plan. TRICARE Referrals and Prior Authorizations.
Otherwise providers must submit all medical documentation directly to the VA Medical Center VAMC supervising the Veterans care. Complete all necessary information in the necessary fillable fields. Tips for creating referrals and authorizations.
The only reason to submit medical documentation to TriWest is for a requested clinical quality review or to support a Secondary Authorization Request SAR where TriWest is scheduling and coordinating care. Use our Prior Authorization Referral and Benefit tool. TriWest Healthcare Alliance is On a Mission to Serve our nations Veterans and military community in partnership with the Department of Veterans Affairs VA in administering the Veterans Choice Program VCP and Veterans Affairs Patient-Centered Community Care PC3 program.
Give the form to your provider to complete and send back to Express Scripts. Non-network providers are encouraged to submit online as electronic requests save time and improve accuracy. If you have a referral then your provider gets prior authorization at the same time.
Be aware there some services require a separate prior authorization review. Check if we offer a Letter of Attestation you can attach instead of clinical. Is it a limited benefit.
Online authorization and referral tools offer quick and easy submission and status tracking of prior authorizations referrals and inpatient and discharge notifications. Preauthorization review is only required for TRICARE For Life TFL beneficiaries when TFL is the primary payer for the specific services listed below. You need to contact your regional contractor for prior authorization.
Avoid extra work and first check if HNFS approval is needed. Inpatient TRICARE Service RequestNotification Form Network providers requesting prior authorization for an elective admission or submitting an inpatient admission notification are required to submit online.
 Triwest Authorization Form Fill Online Printable Fillable Blank Pdffiller
Triwest Authorization Form Fill Online Printable Fillable Blank Pdffiller
 Free 8 Sample Tricare Authorization Forms In Pdf Ms Word
Free 8 Sample Tricare Authorization Forms In Pdf Ms Word
Https Hmsa Com Portal Provider Tricare Authorization List 031507 Tw07 001b Pdf
 Tricare4u Authorization Fill Online Printable Fillable Blank Pdffiller
Tricare4u Authorization Fill Online Printable Fillable Blank Pdffiller
 Free 8 Sample Tricare Authorization Forms In Pdf Ms Word
Free 8 Sample Tricare Authorization Forms In Pdf Ms Word
Https Www Tricare West Com Content Dam Hnfs Tw Prov Resources Pdf Hnfs Parb Tool Guide Pdf
Https Www Tricare West Com Content Dam Hnfs Tw Prov Resources Pdf Hnfs Parb Tool Guide Pdf
 Tricare Appeal Form Pdf Fill Online Printable Fillable Blank Pdffiller
Tricare Appeal Form Pdf Fill Online Printable Fillable Blank Pdffiller
Https Hmsa Com Portal Provider Tricare Patient Referral Authorization Form 0307 Tw07 001c Pdf
 Triwest Authorization Form Fill Online Printable Fillable Blank Pdffiller
Triwest Authorization Form Fill Online Printable Fillable Blank Pdffiller
 Free Tricare Prior Rx Authorization Form Pdf Eforms
Free Tricare Prior Rx Authorization Form Pdf Eforms
Https Www Tricare West Com Content Dam Hnfs Tw Prov Resources Pdf Hnfs Parb Tool Guide Pdf
Https Www Tricare West Com Content Dam Hnfs Tw Prov Resources Pdf December2019 Prov In Case You Missed It Email Pdf
Comments
Post a Comment