Featured
Does Blue Cross Blue Sheild Cover Therapy
Applied behavior analysis or ABA Physical speech and occupational therapy. And The Dental Network Inc.
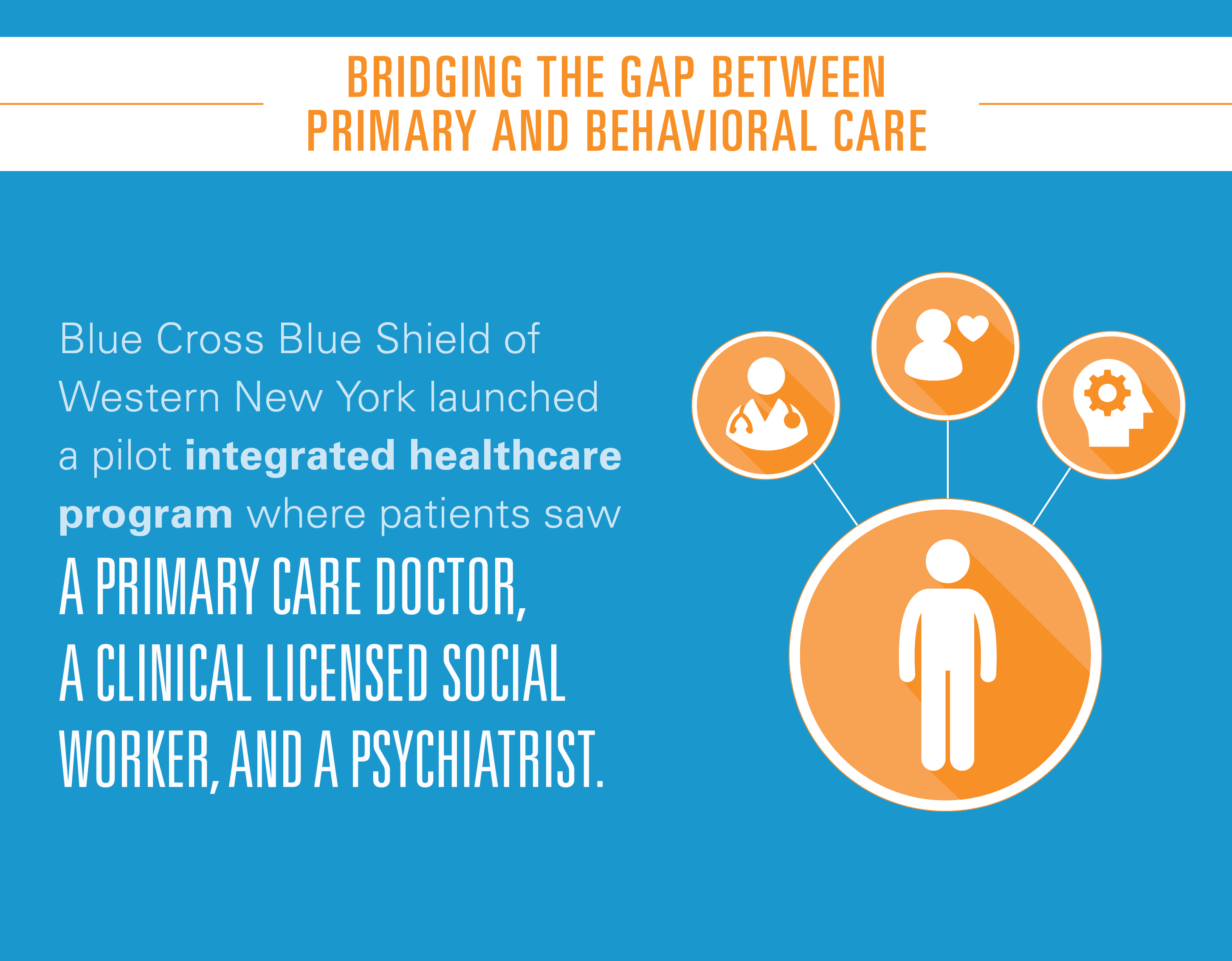 Bright Idea Integrating Behavioral Health With Primary Care Blue Cross Blue Shield
Bright Idea Integrating Behavioral Health With Primary Care Blue Cross Blue Shield
Coverage for Gender Reassignment Surgery.

Does blue cross blue sheild cover therapy. Blue Cross and Blue Shield of Texas BCBSTX gives health care benefits and access to care to help your child stay well. Underwrite products in Maryland only. Standard autism benefits include.
Speech Therapy services ARE NOT ELIGIBLE FOR COVERAGE for any of the following. Browse our extensive directory of the best BlueCross andor BlueShield Massage Therapists and BlueCross andor BlueShield Massage near you. Routine physicals for children from birth through 20 years of age.
Guidelines for getting help. BLUE CROSS BLUE SHIELD and the Cross and Shield Symbols are registered service marks of the Blue Cross and Blue Shield Association an association of independent Blue Cross and Blue Shield Plans. In most instances the benefit for Massachusetts managed care group members is 60 visits per member per calendar year.
Heres how to get those services and find out what services are included in your benefits. Coverage for Transgender Services. Washington The Blue Cross and Blue Shield BCBS Government-wide Service Benefit Plan also known as the Federal Employee Program FEP is partnering with AbilTo Inc the nations largest remote behavioral change therapy company to offer certain federal employees access to innovative programs that will empower FEP members to live healthier lives.
Coverage for Gender Reassignment Surgery. 90801 15360 90801 diagnostic Evaluation 90806 9005 90806 45-50 minute psychotherapy session 90847 10569 90847 family therapy with patient present couples counseling 90846 8433 90846 family therapy without patient present. BCBSTX covers all medically necessary care that Medicaid covers.
Primary care providers PCPs and designated specialists with an open referral from the PCP can refer a member for short-term rehabilitation therapies including. The Blue Cross and Blue Shield Association does not intend by the FEP Medical Policy Manual or by any particular medical policy to recommend advocate encourage or discourage any particular medical technologies. Blue Care Network plans cover or help pay for mental health and substance use disorder services.
Supply is medically necessary does not constitute a representation or warranty that the Blue Cross and Blue Shield Service Benefit Plan covers or pays for this service or supply for a particular member. Blue Cross Blue Shield of North Carolina. Waiving cost-sharing for COVID-19 testing and treatment.
Blue Cross Blue Shield of Massachusetts. Waiving all prior authorization requirements for COVID-19 testing and related covered services. Anthem Blue Cross Blue Shield.
Coverage for Gender Reassignment Surgery. CareFirst of Maryland Inc. FEP 80152 Orthopedic Applications of Stem Cell Therapy Including Allografts and Bone Substitutes Used With Autologous Bone Marrow.
Services Your Plan Generally Does NOT Cover Check your plans FEHB brochure for more information and a list of any other excluded services Cosmetic surgery Private-duty nursing Infertility treatment Routine eye care Adult Long-term care Weight loss programs Other Covered Services Limitations may apply to these services. Remember the Preferred Medical Doctor. Dysfunctions that are self-correcting such as language therapy for young children with natural dysfluency or developmental articulation errors services which maintain function by using routine repetitive and reinforced procedures that are neither diagnostic or.
That means members will pay nothing out-of-pocket to take care of their COVID-19-related health needs. The therapy must be received by Blue Cross. Browse our extensive directory of the best BlueCross and BlueShield Therapists BlueCross and BlueShield Psychologists and BlueCross and BlueShield Counselors near you.
Increasing access to prescription medications. Theyre part of your behavioral health coverage. 13 Zeilen As a Blue Cross Community Health Plans member you have access to medical.
Visits to PCPs specialists with an OK ahead of time for out-of-network providers or other providers. Most Blue Cross plans cover or help pay for services that treat autism spectrum disorders for members through the age of 18. Medical decisions relative to medical technologies are to be made strictly by memberspatients in consultation with their health care providers.
 Does Insurance Cover Therapy When How To Check And More Tips
Does Insurance Cover Therapy When How To Check And More Tips
 Blue Cross Blue Shield Cpap Therapy Policies Health Sqyre
Blue Cross Blue Shield Cpap Therapy Policies Health Sqyre
 Blue Cross Blue Shield Waives Cost Sharing Fees For Psychotherapy And Counseling Telehealth Visits Due To Covid 19 Steven J Hanley Ph D
Blue Cross Blue Shield Waives Cost Sharing Fees For Psychotherapy And Counseling Telehealth Visits Due To Covid 19 Steven J Hanley Ph D
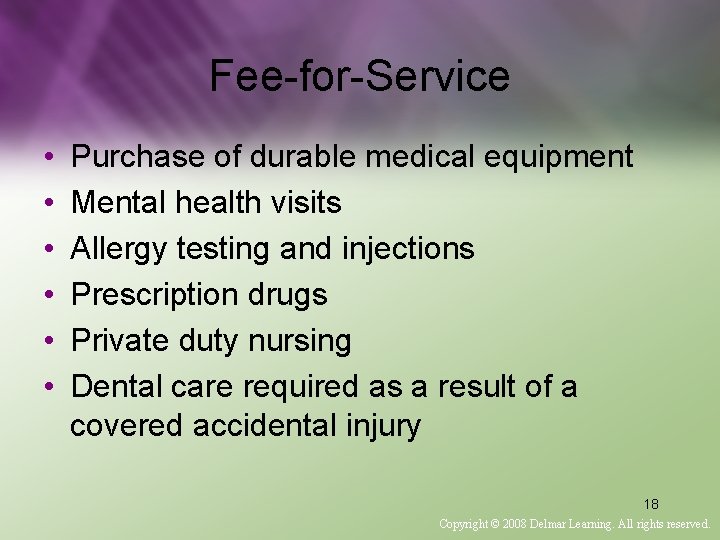
 Insurance Reimbursement Rates For Psychotherapy 2020
Insurance Reimbursement Rates For Psychotherapy 2020
 Blue Cross Blue Shield For Therapy Zencare Guide Zencare
Blue Cross Blue Shield For Therapy Zencare Guide Zencare
 Petition Blue Cross Blue Shield Cover Speech Therapy For Children With Down Syndrome Change Org
Petition Blue Cross Blue Shield Cover Speech Therapy For Children With Down Syndrome Change Org
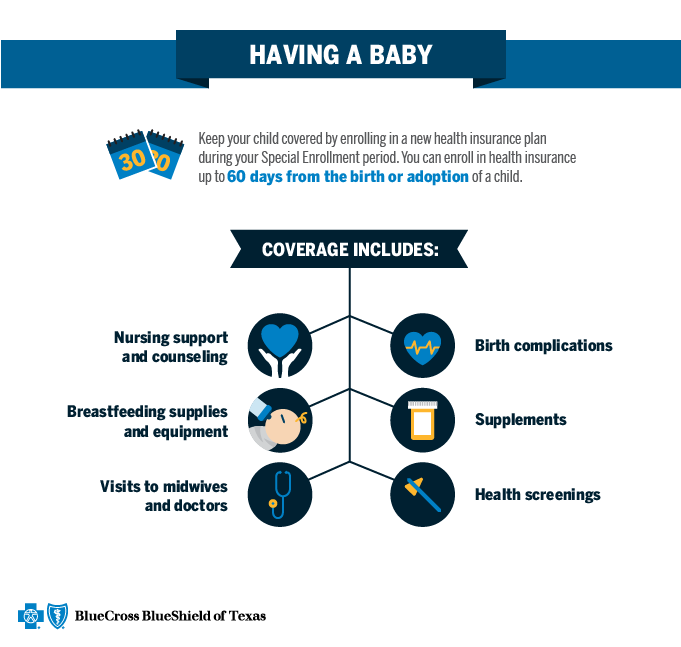 Qualifying Event Baby Blue Cross And Blue Shield Of Texas
Qualifying Event Baby Blue Cross And Blue Shield Of Texas
 Does Blue Cross Blue Shield Cover Therapy Drug Rehab
Does Blue Cross Blue Shield Cover Therapy Drug Rehab
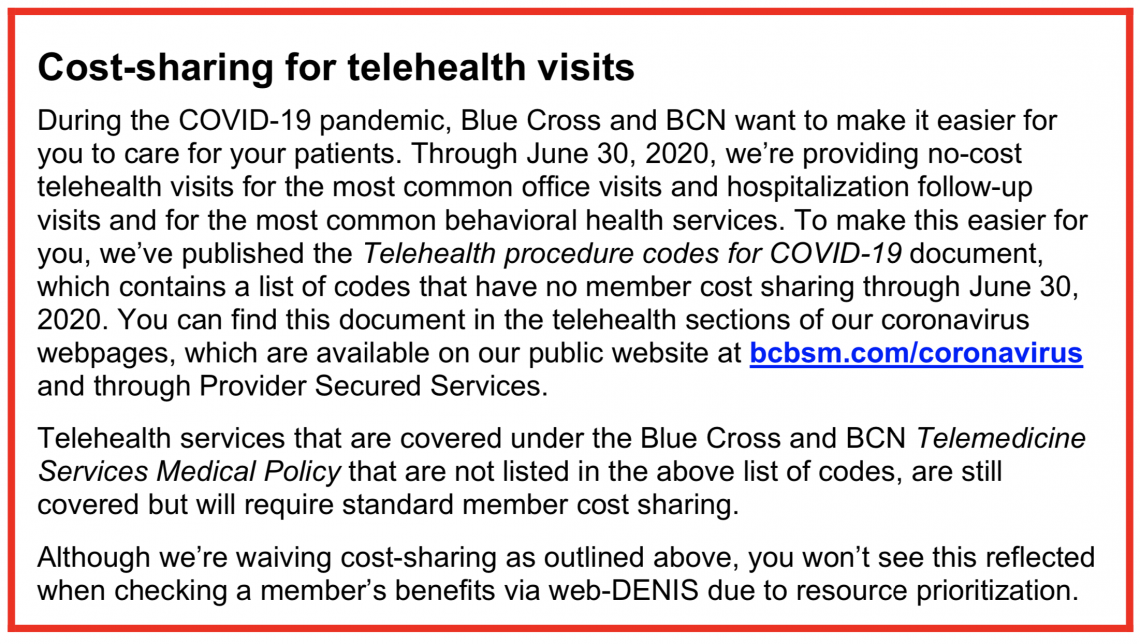 Blue Cross Blue Shield Waives Cost Sharing Fees For Psychotherapy And Counseling Telehealth Visits Due To Covid 19 Steven J Hanley Ph D
Blue Cross Blue Shield Waives Cost Sharing Fees For Psychotherapy And Counseling Telehealth Visits Due To Covid 19 Steven J Hanley Ph D
Blue Cross Blue Shield Wellspring Counseling
 Petition Blue Cross Blue Shield Cover Therapy Treatments For Reed Change Org
Petition Blue Cross Blue Shield Cover Therapy Treatments For Reed Change Org
 Blue Cross Blue Shield For Therapy Zencare Guide Zencare
Blue Cross Blue Shield For Therapy Zencare Guide Zencare
 Does Blue Cross Blue Shield Cover Psychiatry
Does Blue Cross Blue Shield Cover Psychiatry
 Blue Cross Blue Shield California Cpap Policies Health Sqyre
Blue Cross Blue Shield California Cpap Policies Health Sqyre
Comments
Post a Comment