Featured
- Get link
- X
- Other Apps
Who Does Prior Authorization
Labs must register their tests to participate as part of the Genetic and Molecular Lab Testing NotificationPrior Authorization process. A prior authorization PA sometimes referred to as a pre-authorization is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine medical device or procedure.
 Charm Ehr Electronic Prior Authorization Epa
Charm Ehr Electronic Prior Authorization Epa
CMS clarified that claims related to or associated with services that require prior authorization as a condition of payment will not be paid if the service requiring prior authorization is also not paid.

Who does prior authorization. A provider or supplier submits either the prior authorization request or pre-claim review request with all supporting medical documentation for provisional affirmation of coverage for the item or service to their Medicare Administrator Contractor MAC. Prior authorizationsometimes called precertification or prior approvalis a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage. Learn more about the Genetic Molecular Lab Testing Notification Prior Authorization Process.
Ordering care providers will complete the notificationprior authorization process online or over the phone. EPAs save time and help patients receive their medications faster. Your insurance company will contact you with the results to let you know if your drug coverage has been approved or denied or if they need more information.
Its an approval of coverage from your insurance company not your doctor. What is a prior authorization. Prior authorization also called prior approval or pre-authorization is a process that many health insurance companies as well as Medicare and Medicaid use to manage costs.
Only associated services performed in the HOPD setting will be affected. Prior authorization is a restriction put in place by insurance companies so they can decide whether or not they will pay for certain medicines. What Does Prior Authorization Mean.
Prior authorization is a requirement that your physician or hospital obtains approval from your health insurance company before prescribing a specific medication for you or performing a particular medical procedure. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. Prior authorization a utilization management UM process used by health insurance companies to determine coverage for a prescribed procedure service or medication is now becoming a mandatory requirement by the vast majority of large insurance companies.
The physician who orders the testing is responsible for obtaining prior authorization for the specialized laboratory test. Without this prior approval your health insurance plan may not pay for your treatment leaving you with the bill instead. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
What is prior authorization. If the physicians office does not obtain the necessary prior authorization prior to the specialized laboratory testing the patient will be responsible for. Who is responsible for obtaining prior authorization.
This significantly higher level of transparency should help reduce repeated requests for prior authorizations thereby lowering costs and the. Prior Authorization Specialists are individuals responsible for the entire process of prior authorization for a client. They manage communication between stakeholders of clients healthcare providers and insurance companies to request for prior authorizations.
Select payers providers and patients will now have electronic access to pending and active prior authorization decisions. Service code if available HCPCSCPT To better serve our providers business partners and patients the Cigna Coverage Review Department is transitioning from PromptPA fax and phone coverage reviews also called prior authorizations to Electronic Prior Authorizations ePAs. Prior authorizations for prescription drugs are handled by your doctors office and your health insurance company.
Prior authorization must be provided before the insurance company will provide full or any coverage for those medications. Prior authorization for prescription drugs is required when your insurance company asks your physician to get specific medications approved by the insurance company. Prior authorization PA is a requirement that your physician obtain approval from your health insurance plan to prescribe a specific medication for you.
Before you can get coverage for certain medications tests procedures surgeries and medical devices you need to get prior authorization. These related services include but are not limited to anesthesiology services physician services andor facility services. Their duties include ensuring complete and updated patient and claim documentation performing daily billings auditing accounts.
 What Is Prior Authorization Why Do Insurance Companies Require It Academic Healthplans
What Is Prior Authorization Why Do Insurance Companies Require It Academic Healthplans
How To Obtain Health Insurance Prior Authorization In 3 Minutes Or Less
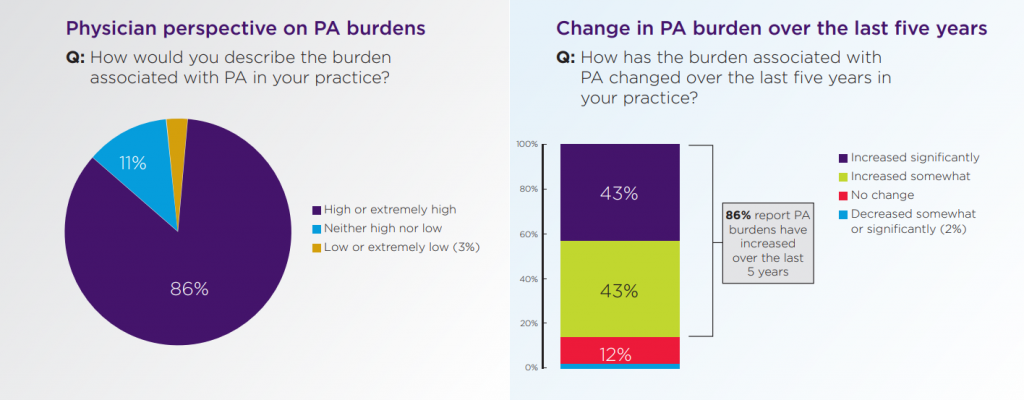
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
 What Is Prior Authorization Prior Authorization Training
What Is Prior Authorization Prior Authorization Training
 The Ultimate Guide To Prior Authorization Myndshft
The Ultimate Guide To Prior Authorization Myndshft
 The Ultimate Guide To Prior Authorization Myndshft
The Ultimate Guide To Prior Authorization Myndshft
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
 Why Automation Is The Key To Fixing Prior Authorization Myndshft
Why Automation Is The Key To Fixing Prior Authorization Myndshft
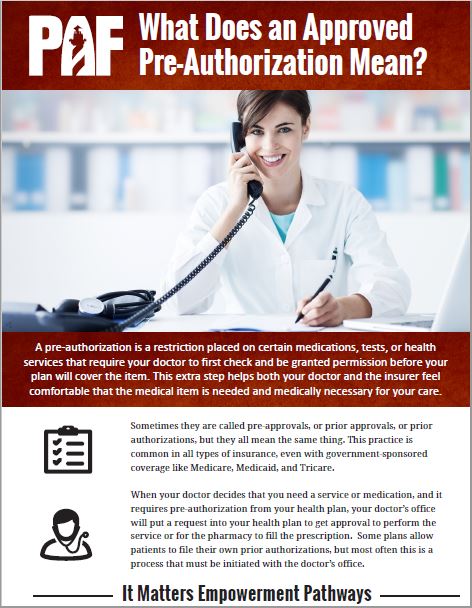 What Does An Approved Pre Authorization Mean Patient Advocate Foundation
What Does An Approved Pre Authorization Mean Patient Advocate Foundation
 Prior Authorization 50 State Network
Prior Authorization 50 State Network
 Prior Authorization Understand It And Simplify It Patients Rising
Prior Authorization Understand It And Simplify It Patients Rising
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
Comments
Post a Comment