Featured
Bcbs Of Mi Prior Authorization Form
Medicare Plus Blue PPO non-Michigan Skilled Nursing Facility Acute Rehabilitation Facility Fax Assessment Form PDF Medicare Plus Blue PPO LTACH Fax Assessment Form PDF. LTACH and Skilled Nursing Facility Enhancement Assessment Form PDF Blue Cross PPO Request for Preauthorization Form PDF Medicare Plus Blue PPO.
Https Www Bcbsm Com Content Dam Public Providers Documents Medical Policy Router Bcbsm Requirements Pdf
Refer to the Blue Cross Musculoskeletal services page for a list of the procedure codes that require authorization from TurningPoint and for more information on how to submit prior authorization requests.

Bcbs of mi prior authorization form. To find a prior authorization form visit our forms page or click on the links below. Medicaid only BCCHP and MMAI. Blue Cross Blue Shield of Michigan Request for Preauthorization Form.
AUTHORIZATION REQUEST FORM Utilization management toll-free phone. Services must be a covered Health Plan Benefit and medically necessary with prior authorization as per Plan policies and procedures. ABA Clinical Service Request Form.
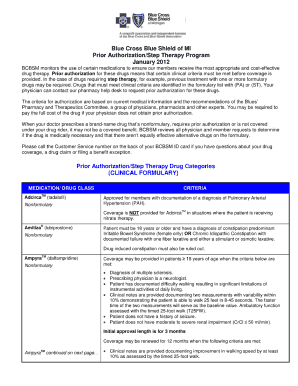
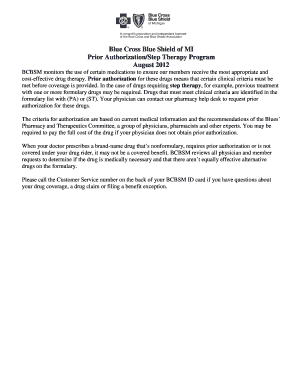
Prior authorization requests are defined as requests for pre-approval from an insurer for specified medications or quantities of medications before they are dispensed. 1-833-217-9670 Utilization management local phone. See Musculoskeletal procedure codes that require authorization by TurningPoint.
Medicaid Claims Inquiry or Dispute Request Form. Prior authorization is required for some membersservicesdrugs before services are rendered to confirm medical necessity as defined by the members health benefit plan. 1 2021 providers should submit prior authorization requests for to TurningPoint.
For ERS or TRS participants refer to specific form links above Form. An authorization is not a guarantee of paymentMember must be eligible at the time services are rendered. This form will be updated periodically and the form number and most recent revision date are displayed in the top left hand corner.
Medicaid only BCCHP and MMAI Medicaid Service Authorization Dispute Resolution Request Form. For dates of service on or after Jan. This form is made available for use by prescribers to initiate a prior authorization request with the health insurer.
Behavioral Health for Other BCBSTX Plans. In order to be able to submit your prior authorization requests electronically you will need to. Fax joint and spine procedures authorization request forms to 313-879-5509.
Member ID including any alpha prefix. Behavioral Health Substance Abuse Continued Stay Review Form. ABA Initial Assessment Request.
Blue Advantage Physician Drug Authorization Request Form. Become a registered web-DENIS user. Applied Behavior Analysis ABA forms.
Behavioral Health Substance Abuse Certification. Form Title Networks Expedited Pre-service Clinical Appeal Form. Skilled nursing facility assessment form PDF for attaching to the case in the e-referral system starting Dec.
Fax pain management authorization request forms to 313-483-7323. Most preauthorization requests can be resolved by contacting Provider Relations and Servicing or PRS and requesting member benefits. Complete this form and fax it to.
If this admission is for an organ transplant and authorization has not been obtained please call the Human Organ Transplant Program department at 1-800-242-3504. Forms Blue Cross PPO commercial Acute Inpatient Fax Assessment Form PDF Acute Rehabilitation and Skilled Nursing Facility Fax Assessment Form PDF for faxing rehabilitation and SNF requests. Non-formulary drugs Part D reviewed by ESI.
Authorization for Disclosure of Mental Health Clinical Information. Use these forms to obtain prior authorization for administering medications in physicians offices and outpatient hospitals including urgent care hospital-based infusion care centers and clinics where the drug is injected or infused and billed on a UB04 or CMS 1500 form. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required.
A prior authorization is not a guarantee of. Prior authorization sometimes called preauthorization or pre-certification is a pre-service utilization management review. Prior authorization requests are defined as requests forpre -approval from an insurer for specified medications or quantities of medications before they are dispensed.
1-866-411-2585 For URMBT fax form to 1-866-915-9811 Include hospital admission HP and PMR consultation notes. For dates of service prior to Jan. Individual and Family Plans.
Behavioral Health Case Management Prescreening. Requests for the following services can be made by fax or mail. However if you would like to submit a request for preauthorization after contacting PRS you may submit a written request by completing this form.
Blue Cross PPO Commercial Forms. 1 2021 authorization is required for lumbar spinal. Blue Advantage Drug Prior Authorization.
313-908-6040 Utilization management fax. 313-879-5509 1 P a g e Todays date and time. Requests can be submitted beginning Dec.
Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
B C B S P R I O R A U T H O R I Z A T I O N F O R M Zonealarm Results
Https Www Bcbsm Com Pdf Wf 12475 Mar 12 Pdf
 Bcn Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Bcn Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Https Www Bcbsm Com Content Dam Public Providers Documents Global Medication Authorization Request Form Pdf
 Blue Cross Blue Shield Of Michigan Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Blue Cross Blue Shield Of Michigan Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
 Pdf Telecharger Bcbs Of Michigan Prior Authorization Form For Dme Gratuit Pdf Pdfprof Com
Pdf Telecharger Bcbs Of Michigan Prior Authorization Form For Dme Gratuit Pdf Pdfprof Com
Http Www Domoa Org Assets Docs 1 Bcbsm Benruss Pdf
 Fillable Online Bcbs Of Michigan Prior Authorization Form Fax Email Print Pdffiller
Fillable Online Bcbs Of Michigan Prior Authorization Form Fax Email Print Pdffiller
Https Www Bcbsm Com Content Dam Public Consumer Documents Help Documents Forms Bcbsm Appeal Form Pdf
Https Www Bcbsm Com Content Dam Public Consumer Documents Help Documents Forms Authorization Use Disclosure Protected Health Information Pdf
Https Www Michigan Gov Documents Difs Fis 2288 501398 7 Pdf
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
 Late Sanction After That Do Something Tread Carefully Cure Programs Blue Cross Blue Shield Of California Prior Authorization Form
Late Sanction After That Do Something Tread Carefully Cure Programs Blue Cross Blue Shield Of California Prior Authorization Form
 Blue Cross Blue Shield Of Michigan Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Blue Cross Blue Shield Of Michigan Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Comments
Post a Comment