Featured
- Get link
- X
- Other Apps
Does Bcbs Cover Counseling
Counseling and if indicated after counseling genetic testing. Sometimes we need to review to be sure the service is medically necessary and.
 Wichita Therapy Accepting Blue Cross Blue Shield Bcbs Fiat Family Services
Wichita Therapy Accepting Blue Cross Blue Shield Bcbs Fiat Family Services
Z803 Z8041 Z853 Z8543 Procedure code 96040 is reimbursable as preventive when submitted with one of the following primary diagnosis codes.

Does bcbs cover counseling. The Committee has issued separate papers on a number of related topics in the area of credit risk including credit risk modelling and credit risk management. Call Member Services at 1-877-860-2837 TTYTDD. The type of service you might need depends on your personal situation.
Interact with a banks overall credit risk practices and regulatory framework but does not endeavour to set out regulatory capital requirements on expected loss provisioning under the Basel capital framework. Before getting mental health care counseling or substance use disorder services call the behavioral or mental health preauthorization number on the back of your Blue Cross ID card. For supervision of clinical work with patients you need to follow the requirements set out by your state-issued license or registration.
Does the BCN requirements document cover supervision. Theyre part of your behavioral health coverage. Well help you get the information you need.
Please confirm when you make an appointment that. If you want to know if youre a carrier of the BRCA12 gene talk to your doctor about genetic counseling. They include BC BS Therapists in Tennessee BCBS psychologists and bcbs counseling.
When we review your services that doesnt guarantee payment of your claims. You must also receive prior approval from us. If eligible you must receive genetic counseling and evaluation services before you receive preventive BRCA testing.
Masters LICSW LMFT LMHC 90801 12309. Couples Counseling Associates is connected to Blue Cross Blue Shield PPO. 711 and we can help you find out what services are covered.
Steps previously taken by BCBS companies include. While many Blue Cross Blue Shield policies provide a range of benefits to cover addiction treatment options and programs vary depending on the state you reside in and your individual plan. Blue Care Network members under age 65.
Behavioral health services can help those facing mental health conditions substance abuse or a behavioral health crisis. Yes but only for billing purposes. The vast majority of Blue Cross Blue Shield insurance plans cover therapy.
90801 15360 90801 diagnostic Evaluation 90806 9005 90806 45-50 minute psychotherapy session 90847 10569 90847 family therapy with patient present couples counseling 90846 8433 90846 family therapy without patient present BCBS. Adult physicals and blood pressure and cholesterol screenings. As individuals in the United States are being diagnosed with COVID-19 Coronavirus we recognize BlueCross BlueShield of Western New York members may have concerns.
Eligible candidates will meet with a genetic counselor to discuss the risks limitations and. Please confirm when you make an appointment that. Heres how to get those services and find out.
Does bcbs cover couples counseling Does insurance cover couples therapy. The treatment providers listed above report that their addiction treatment services are covered by Blue Cross Blue Shield. This includes the minimum number of supervision hours the proximity of the.
We offer free invoicing to all other insurance companies at the end of the network. You do not need a referral for a provider. To talk with a counselor.
This page answers frequently asked questions about insurance reimbursements for couples therapy. The same number you call for medical and mental health benefits questions. Youll need to be sure that your plan covers your health care services and that your coverage is active at the time you receive treatment.
Z803 or Z8041 All other procedure codes for BRCA are payable with a diagnosis in Diagnosis List 1. You can get help with a mental health or substance use issue 24 hours a day seven days a week. If however your plan started before 2014 when the Affordable Care Act was enacted your plan may not cover therapy.
If you or your covered dependent are in a crisis situation call 800 252-8039 TTY711. Physical speech and occupational therapy. If you dont get prior authorization when its needed we might not pay your claim.
Blue Care Network plans cover or help pay for mental health and substance use disorder services. You wont pay a copay or coinsurance for these services and you dont need to meet your deductible before you use these services. While the situation is fluid and information is being updated daily one thing that will remain constant is our commitment to connecting our members to the care they need.
Covering full costs of medically necessary diagnostic tests related to COVID-19 waiving of prior authorizations for diagnostic tests and covered services for members if diagnosed with COVID-19 increased access to prescription medications and expanded access to telehealth and nurseprovider hotlines. All plans also offer preventive services at no charge. They include BC BS Therapists in South Carolina BCBS psychologists and bcbs counseling.
All Blue Care Network HMO plans require preauthorization.
 Increasing Access To Behavioral Healthcare In The Face Of Covid 19 Blue Cross Blue Shield
Increasing Access To Behavioral Healthcare In The Face Of Covid 19 Blue Cross Blue Shield
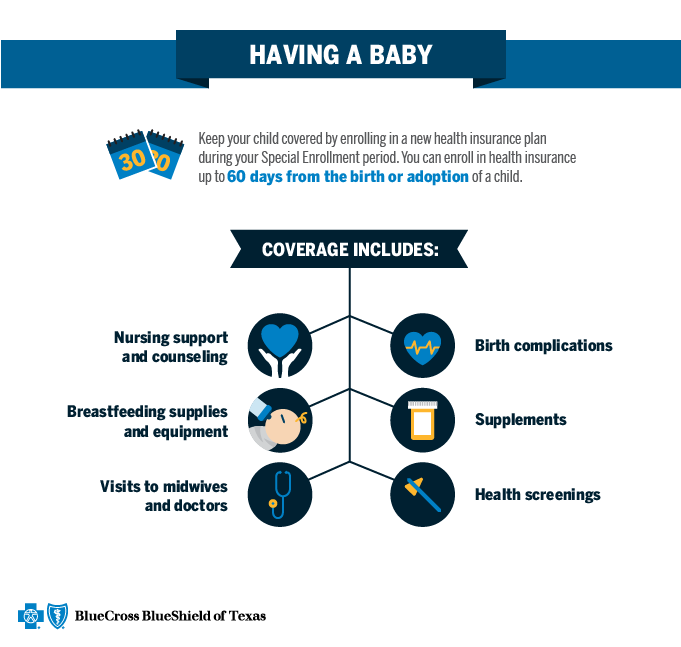 Qualifying Event Baby Blue Cross And Blue Shield Of Texas
Qualifying Event Baby Blue Cross And Blue Shield Of Texas
 Health Plan Overview Blue Cross And Blue Shield S Federal Employee Program
Health Plan Overview Blue Cross And Blue Shield S Federal Employee Program
 Insurance Reimbursement Rates For Psychotherapy 2020
Insurance Reimbursement Rates For Psychotherapy 2020
 Blue Cross Blue Shield For Therapy Zencare Guide Zencare
Blue Cross Blue Shield For Therapy Zencare Guide Zencare
 Does Blue Cross Blue Shield Cover Therapy Drug Rehab
Does Blue Cross Blue Shield Cover Therapy Drug Rehab
 Marital Therapy Counseling Psychotherapy I Raleigh Durham Nc
Marital Therapy Counseling Psychotherapy I Raleigh Durham Nc
 Blue Cross Blue Shield For Therapy Zencare Guide Zencare
Blue Cross Blue Shield For Therapy Zencare Guide Zencare
 Blue Cross Blue Shield Waives Cost Sharing Fees For Psychotherapy And Counseling Telehealth Visits Due To Covid 19 Steven J Hanley Ph D
Blue Cross Blue Shield Waives Cost Sharing Fees For Psychotherapy And Counseling Telehealth Visits Due To Covid 19 Steven J Hanley Ph D
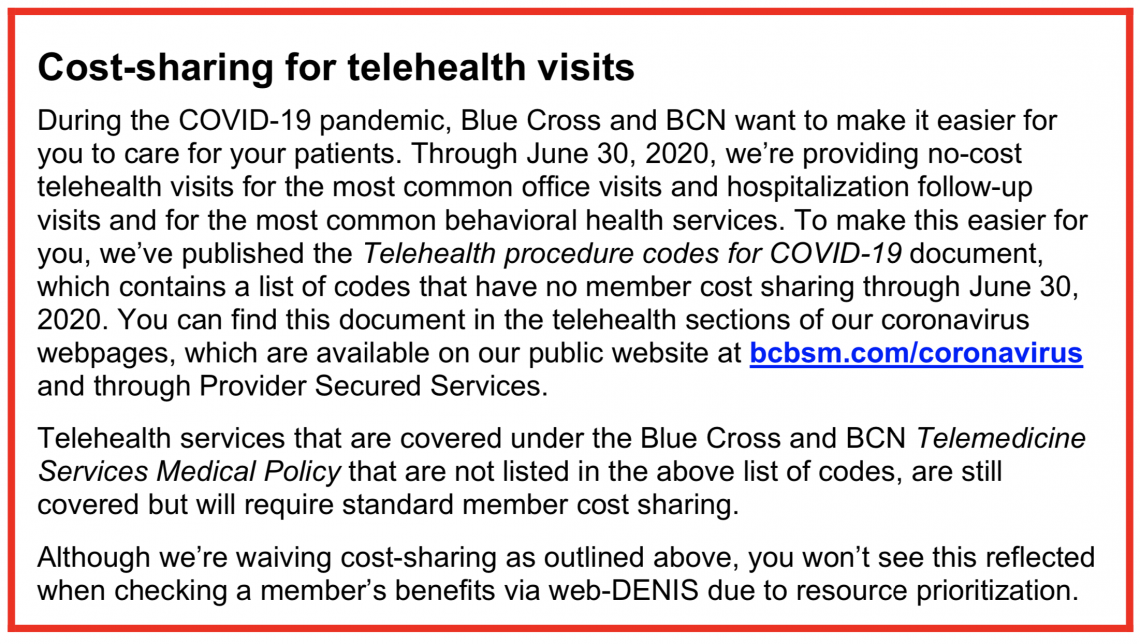 Blue Cross Blue Shield Waives Cost Sharing Fees For Psychotherapy And Counseling Telehealth Visits Due To Covid 19 Steven J Hanley Ph D
Blue Cross Blue Shield Waives Cost Sharing Fees For Psychotherapy And Counseling Telehealth Visits Due To Covid 19 Steven J Hanley Ph D
Https Www Bcbsal Org Web Documents 1512426 17902664 Adt Behavioral Health Flier Print Pdf Aee391f3 B9d9 4cde B5f3 Ce10e8d0b3cd
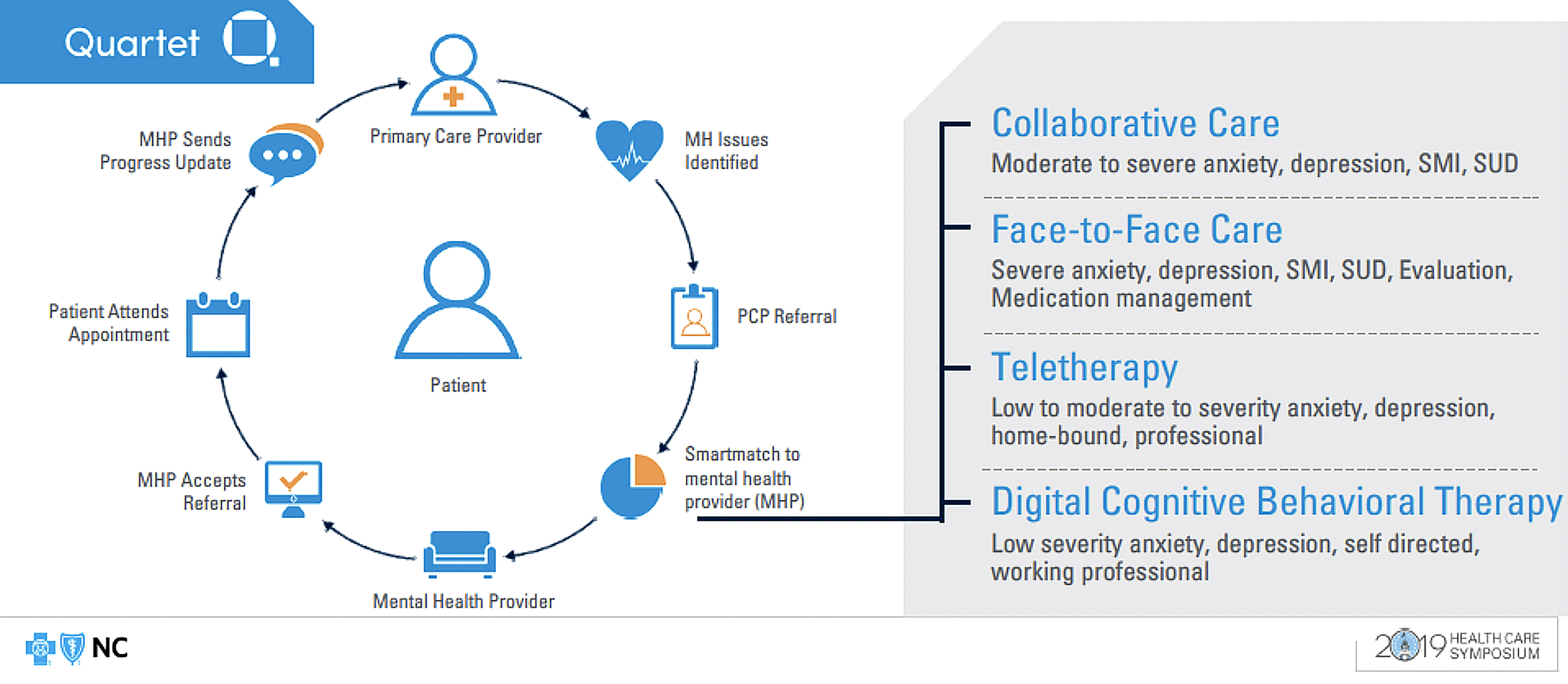 Connecting The Dots A Full Health Approach To Integrated Care Blue Cross Blue Shield
Connecting The Dots A Full Health Approach To Integrated Care Blue Cross Blue Shield
 Does Bcbs Cover Grief Counseling
Does Bcbs Cover Grief Counseling

Comments
Post a Comment