Featured
- Get link
- X
- Other Apps
Anthem Prolia Prior Authorization Form
Individual has had at least one osteoporotic minimal trauma fracture. Prior Authorization Generic Fax Form PDF 173 KB Prior Authorization Urgent Expedited Fax Form PDF 126 KB Tier Exception PDF 109 KB Prescription drug prior authorization and step therapy exception request forms.
Https Www Anthem Com Provider Noapplication F0 S0 T0 Pw E174364 Pdf Na Pharminfo
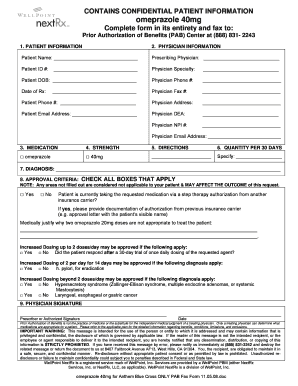
Complete form in its entirety and fax to.
Anthem prolia prior authorization form. Request is for Prolia treatment of bone loss in an adult woman greater than or equal to 18 years of age receiving adjuvant aromatase inhibitor therapy for breast cancer. If you do not obtain prior approval there may be. Reside in the state of Colorado andor Whose prescription drug coverage was sold in the state of Colorado.
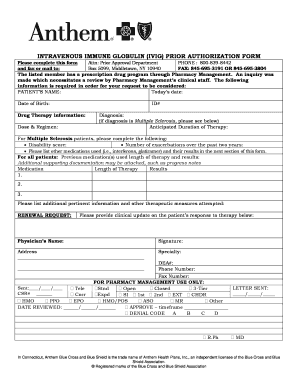
Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Anthem has also made available a series of forms. Office drugs prior authorization request PDF 301 KB Home Self-Administered Injectable Drug authorization request PDF 288 KB.
More forms can be found in the Clinical Pharmacy and Specialty Drugs Prior Authorization Programs section. Provider Forms Guides. For your convenience there are 3 ways to complete a Prior Authorization request.
Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. ICR offers a fast efficient way to securely submit prior authorization requests with clinical documentation. Prior Authorization of Benefits Center at 800 601- 4829.
Prolia Xgeva denosumab Injectable Aetna Precertification Notification 503 Sunport Lane Orlando FL 32809 Medication Precertification Request Phone. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. Members who are speec h- or hearing-im pair ed sh ould call 1 -800-22 1-6915 TD DT TY M onday to Friday 830 a m.
Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its required. Cultural and Linguistic Referral Form. Prolia NTL PAB Fax Form 070715doc.
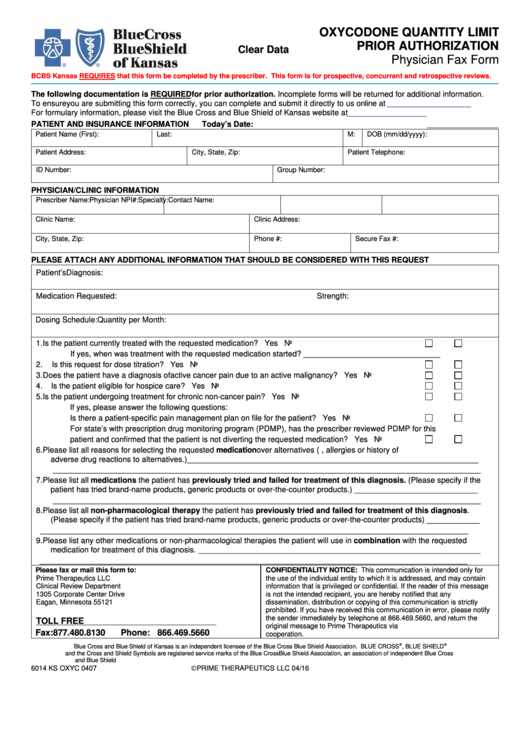
Use these forms to obtain prior authorization for administering medications in physicians offices and outpatient hospitals including urgent care hospital-based infusion care centers and clinics where the drug is injected or infused and billed on a UB04 or CMS 1500 form. Request or Refusal for Interpreter Service Form Armenian. Colorado authorization form The use of this form is mandated for prior authorization requests concerning commercial fully insured members who.
You can also check status of an existing request and auto-authorize more than 40. Service Benefit Plan Prior Approval PO. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost.
Prior Authorization can ensure proper patient selection dosage drug administration and duration of selected drugs. Box 52080 MC 139 Phoenix AZ 85072-2080 Attn. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan.
Please check all that apply. And o Authorization is for no more than 12 months. _____ PATIENT ID.
Member Information required Provider Information required Member Name. Attached is a Prior Authorization request form. Prolia denosumab Prior Authorization of Benefits PAB Form.
Xgeva denosumab Xgeva is proven for the prevention of skeletal-related events in patients with multiple myeloma and with bone. Peer to Peer Scheduling Request Form - UnitedHealthcare offers the opportunity for your physician to speak with our medical director to discuss the medical policy and documentation requirements which determined the response for your prior authorization or concurrent review request. O Prolia dosing is in accordance with the United States Food and Drug Administration approved labeling.
Request or Refusal for Interpreter Service Form Chinese. _____ Bone Loss due to medication. This is called prior approval precertification or preauthorization.
Prolia Prior Authorization Request Form Page 1 of 2 DO NOT COPY FOR FUTURE USE. We review them to ensure they are medically necessary. We are currently in the process of enhancing this forms library.
Certain medical services and treatments need approval before you receive care. FORMS ARE UPDATED FREQUENTLY AND MAY BE BARCODED. During this time you can still find all forms and guides on our legacy site.
1-866-752-7021 Page 2 of 3 FAX. Maximum dosing of 60 mg every 6 months. PA Forms for Physicians When a PA is needed for a prescription the member will be asked to have the physician or authorized agent of the physician contact our Prior Authorization Department to answer criteria questions to determine coverage.
Prolia FEP CSU_MD Fax Form Revised 5312019 Send completed form to. Recommends submitting prior authorization requests for Anthem HealthKeepers Plus members via Interactive Care Reviewer ICR a secure Utilization Management tool available in Availity. 1-888-267-3277 All fields must be completed and legible for precertification review For Medicare Advantage Part B.
Easily find and download forms guides and other related documentation that you need to do business with Anthem all in one convenient location. Request or Refusal for Interpreter Service Form Arabic. To 5 pm Eastern tim e.
Specialist as primary care provider request form.
Https Www11 Anthem Com Ca Provider F1 S0 T0 Pw E229275 Pdf Refer Provider
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Https Www Anthem Com Provider Noapplication F4 S6 T0 Pw E213404 Pdf Refer Ahpprovider State Ct
 Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
 Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
 Fillable Online Anthem Prior Authorization Form For Procedures Fax Email Print Pdffiller
Fillable Online Anthem Prior Authorization Form For Procedures Fax Email Print Pdffiller
 Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
Https Www Anthem Com National Noapplication F1 S0 T0 Pw E232644 Pdf Refer Ahpprovider
 Fillable Online Anthem Prior Auth Request For Form Fax Email Print Pdffiller
Fillable Online Anthem Prior Auth Request For Form Fax Email Print Pdffiller
Https Www Anthem Com Provider Noapplication F1 S0 T0 Pw Ad080665 Pdf Refer Ahpprovider
 Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Https Www Anthem Com Provider Noapplication F1 S0 T0 Pw E244322 Pdf Refer Ahpprovider
Https Www Anthem Com Ca Provider F3 S1 T4 Pw E224354 Pdf Refer Agent
Comments
Post a Comment