Featured
- Get link
- X
- Other Apps
Prior Authorization Website
Prior authorization is designed to help prevent you from being prescribed medications you may not need those that could interact dangerously with others you may be taking or those that are potentially addictive. Alliant Health Solutions has.
 Online Prior Authorization For Medical Services Youtube
Online Prior Authorization For Medical Services Youtube
Under pre-claim review the provider or supplier submits the pre-claim review request and receives the decision prior to claim.
Prior authorization website. Prior authorization is a health plan cost-control process that requires providers to qualify for payment by obtaining approval before performing a service. Customs and Border Protection. It is overused costly inefficient opaque and responsible for patient care delays.
As part of this effort we retired certain fax numbers for medical prior authorization requests in 2019 and asked you to use the Prior Authorization and Notification tool on Link the same website you use to check eligibility and benefits manage claims and update your demographic information. A prior authorization PA sometimes referred to as a pre-authorization is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine medical device or procedure. We use it to make sure your prescription drug is.
On this web page you will find training offerings user manuals review reference materials and links to other training resources. Under prior authorization the provider or supplier submits the prior authorization request and receives the decision prior to rendering services. Official ESTA Application Website US.
Patient Health and Safety. Use the new Novologix online prior authorization PA system to request a PA. Prior authorizationsometimes called precertification or prior approvalis a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
Service code if available HCPCSCPT To better serve our providers business partners and patients the Cigna Coverage Review Department is transitioning from PromptPA fax and phone coverage reviews also called prior authorizations to Electronic Prior Authorizations ePAs. COVID-19 Prior Authorization and Ongoing Patient Care Updates REDIRECT. The Prior Authorization Referral and Benefit Tool allows you to easily determine if an approval from Health Net Federal Services LLC HNFS is required.
Without this prior approval your health insurance provider may not pay for your medication or operation leaving you with the bill instead. A self-service experience and access to real-time status updates. CMS believes prior authorization for certain hospital OPD services will ensure that Medicare beneficiaries continue to receive medically necessary care while protecting the Medicare Trust Fund from improper payments and at the same time keeping the medical necessity documentation requirements unchanged for providers.
If youre not required to get referrals you should know what services need prior authorization. An efficient intake process through a web-based application. Its also a way for your health insurance company to manage costs for.
Were taking a number of steps to reform prior authorization this year. Prior authorization is a requirement that your physician obtains approval from your healthcare provider before prescribing a specific medication for you or to performing a particular operation. Prior Authorization Prior authorization is a routine process.
Support for health care professionals and members affected by severe weather and other emergencies. 05072020 UnitedHealth Group Provides Over 15 Billion of Additional Support in Response to COVID-19 Challenges. Instant approvals for many of your submissions new for 2020 When to use Novologix.
Medically necessary To be medically necessary means it is appropriate reasonable and adequate for your condition. Getting prior authorization means youre getting the care approved by your regional contractor before you actually go to an appointment and get the care. You may need prior authorization for your prescription if it.
Simply select the beneficiarys TRICARE plan option for example TRICARE Prime or TRICARE Prime Remote the beneficiary type for example active duty service member servicing provider type for example network or non-network and the. Help continue our promise to Make America Great Again. Der kostenlose Service von Google übersetzt in Sekundenschnelle Wörter Sätze und Webseiten zwischen Deutsch und über 100 anderen Sprachen.
EPAs save time and help patients receive their medications faster. Alliant Health Solutions offers a variety of training resources to educate the Medicaid Provider community regarding the Prior Authorization PA submission process prior authorization and waiver review process and other review policies and procedures. Prior authorization and pre-claim review are similar but differ in the timing of the review and when services may begin.
If you have a referral then your provider gets prior authorization at the same time.
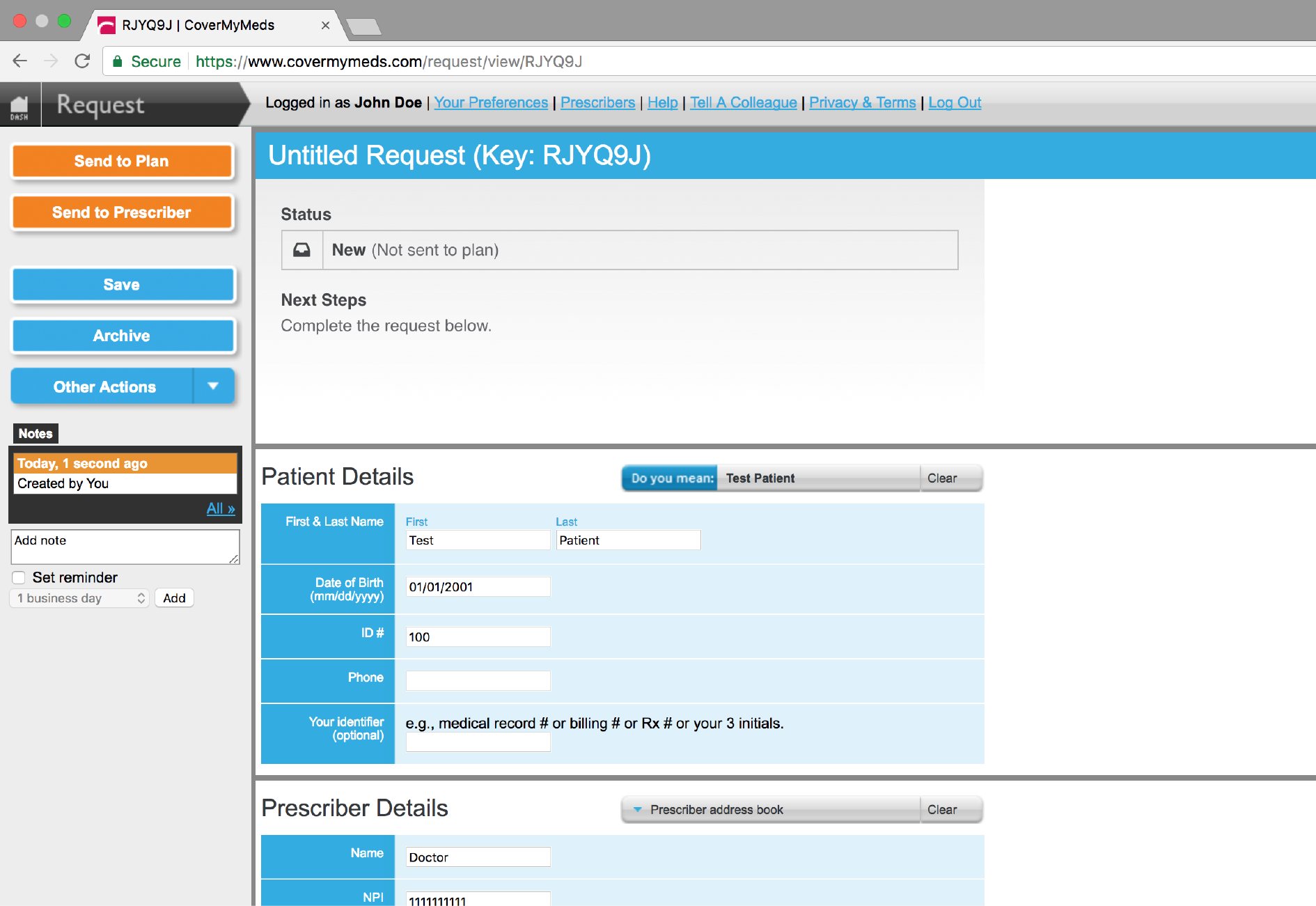 Prior Authorization Forms Covermymeds
Prior Authorization Forms Covermymeds
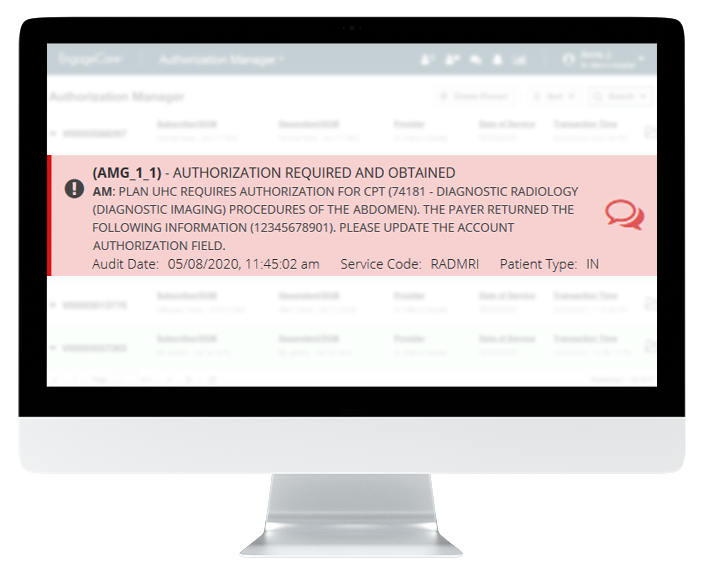 Prior Authorization Software Accureg
Prior Authorization Software Accureg
Https Www Firstcare Com Firstcare Media First Care Pdfs Medicaid Chip Tx Standard Pa Form Rx 201506 Pdf
 How To Obtain Prior Authorizations Jdrf
How To Obtain Prior Authorizations Jdrf
 How To Speed Up Prior Authorization
How To Speed Up Prior Authorization
 Electronic Prior Authorization For Faster Approvals Surescripts
Electronic Prior Authorization For Faster Approvals Surescripts
Https Www Pahealthwellness Com Content Dam Centene Pennsylvania Pdfs Priorauthreqgeneral 20pahw Pdf
 Review Of 2019 Top Prior Authorization Solution Availity
Review Of 2019 Top Prior Authorization Solution Availity
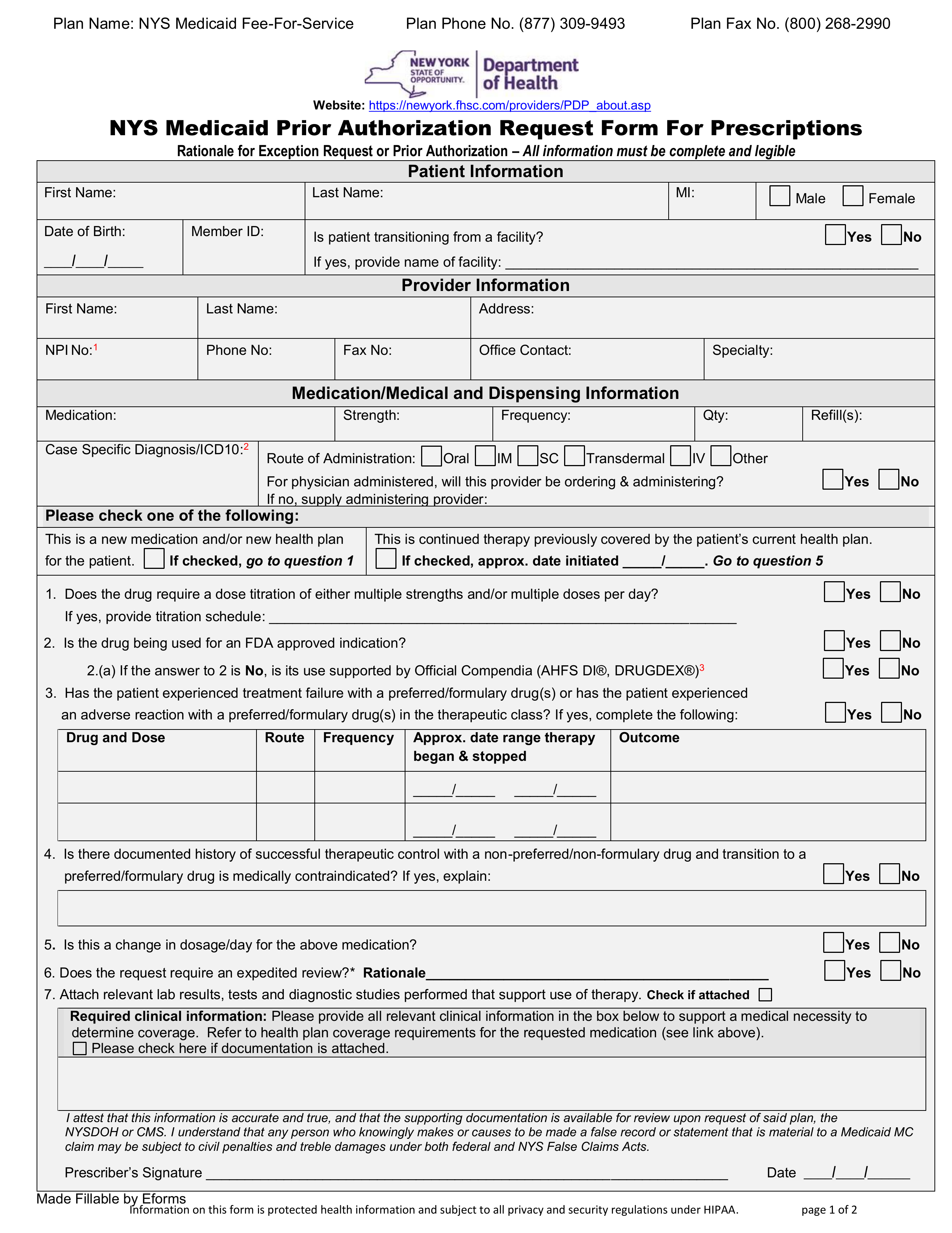 Free New York Medicaid Prior Authorization Form Pdf Eforms
Free New York Medicaid Prior Authorization Form Pdf Eforms

Https Www Azahcccs Gov Resources Downloads Dfmstraining 2018 Patrainingfinalrevised Pdf
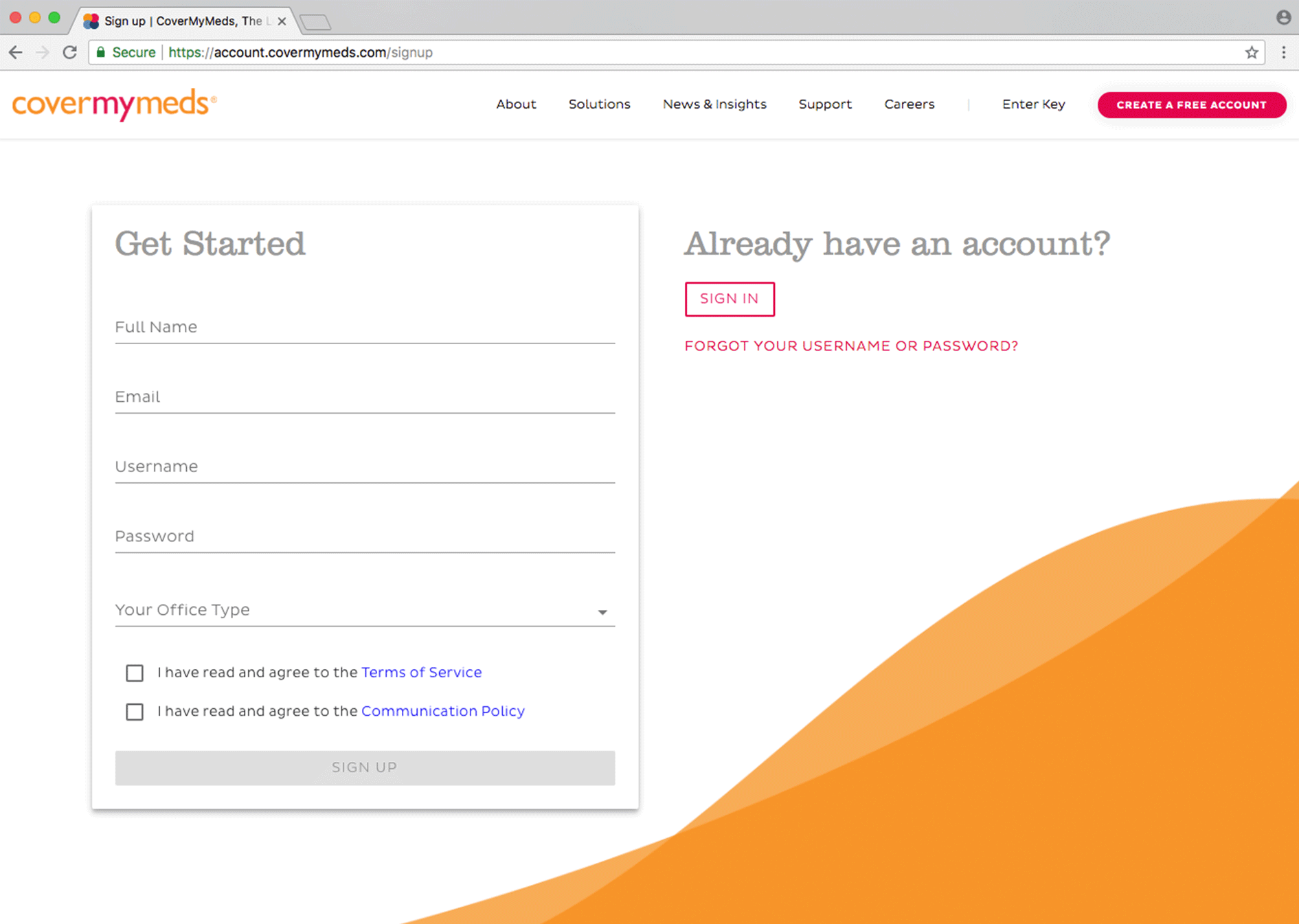 Prior Authorization Forms Covermymeds
Prior Authorization Forms Covermymeds
 Review Of 2019 Top Prior Authorization Solution Azalea Health
Review Of 2019 Top Prior Authorization Solution Azalea Health

Comments
Post a Comment