Featured
- Get link
- X
- Other Apps
Provider Credentialing Application
Beacon Health Contact Information Form fillable Use this form to advise and update Beacon Health about the various staff at the practice or facility and their roles so that we can contact the correct staff for any issue. Health History form and documentation.
 Provider Enrollment Credentialing
Provider Enrollment Credentialing
I have a current application on CAQH.
Provider credentialing application. Here is all important things to care about while compeleting your medicare provider enrollment application in 2021. One reason the process takes so long is that one of the. Rev 102318 3 Provider Practitioner CREDENTIALING APPLICATION If more space than is provided on this Application is needed in order to answer a question completely please use the attached Explanation Form as necessary.
Copy of Malpractice Face sheet. The effective date will be the date the enrollment packet. This requires contacting a range of organizations including medical schools licensing boards and other entities to verify that the providers have the correct licenses and certificates.
This is step by step guide which also talks about various closely related issues regarding medicare provider enrollments. The process that a health insurance carrier assesses a providers qualification and competency is called Provider Credentialing. You will begin the credentialing process by registering with OneHealthPort ProviderSource.
Once Alliance receives a completed credentialing enrollment packet the provider will receive an email from Provider Network Operations stating that the application has been accepted. To set up contracted providers that do not require full credentialing review but where billing for their services will be under the individual provider name. Click here to learn whats needed to become a VSP Network Provider and to see VSPs credentialing policy.
The Credentialing Committee chaired by the Medical Director or their physician designee approve the credentialing application which will allow the provider to become a member of the DWIHN Provider Panel. This form requires personal information education and training information licensure and other professional information in detail. To apply for UMR insurance credentialing you have to apply to the United Healthcare Network.
I have an NPI number. Provider Credentialing Application This Secure Form. This secure form is used to gather information about you so that DBN can provide credentialing services to your facility.
An Overview of the Process. If youre not currently active with CAQH and would like to be a VSP Provider get started here. You can complete a credentialing application through either CAQH ProView or through the Minnesota Credentialing Collaborative.
UMR insurance credentialing is essential if a provider seeks to tap into the client base held by United Healthcare throughout America. Credentialing Credentialing Privileging Application and Hiring Process 6 90-120 days. For providers in Minnesota.
Organizational Provider Credentialing Application Professional liability coverage Attach certifcate showing policy number coverage amounts efective date and expiration date. So lets check out the process for UMR Insurance Provider Credentialing. Any provider who has submitted an application has the ri ght to be informed of the status and to review the application and any information submitted in support of the application.
May 10 2021 This article guides you on how to complete your medicare provider enrollment application in 2021. Fully completed MN Uniform Credentialing Application OR Update Application. For providers in Washington.
Review and approval of the clinicians credentialing application follows the same steps above. To begin credentialing with HealthPartners or adding privileges at a new hospitalentity. Provider credentialing is very time-consuming and usually takes from about six months to a year to complete.
LPs will not be added to Alpha for billing until the credentialing application is approved by Provider Network Credentialing Committee. IDENTIFYING INFORMATION Please provide the practitioners full legal name. Hospital Attestation Secondary Interests Disclosure form and Designated Physician.
This would include any information received by the Beacon Network Management Department while completing primary source verification. Provider credentialing is the process of establishing that medical providers have proper qualifications to perform their jobs. The forms are posted below for your convenience.
It does not how ever include review of any peer review. Providers in the states listed below may use their states form in place of the MultiPlan form for initial credentialing when applying to join our networks or for recredentialing purposes.
Credentialing Process Five Steps To Easy Physician Credentialing Learning Center
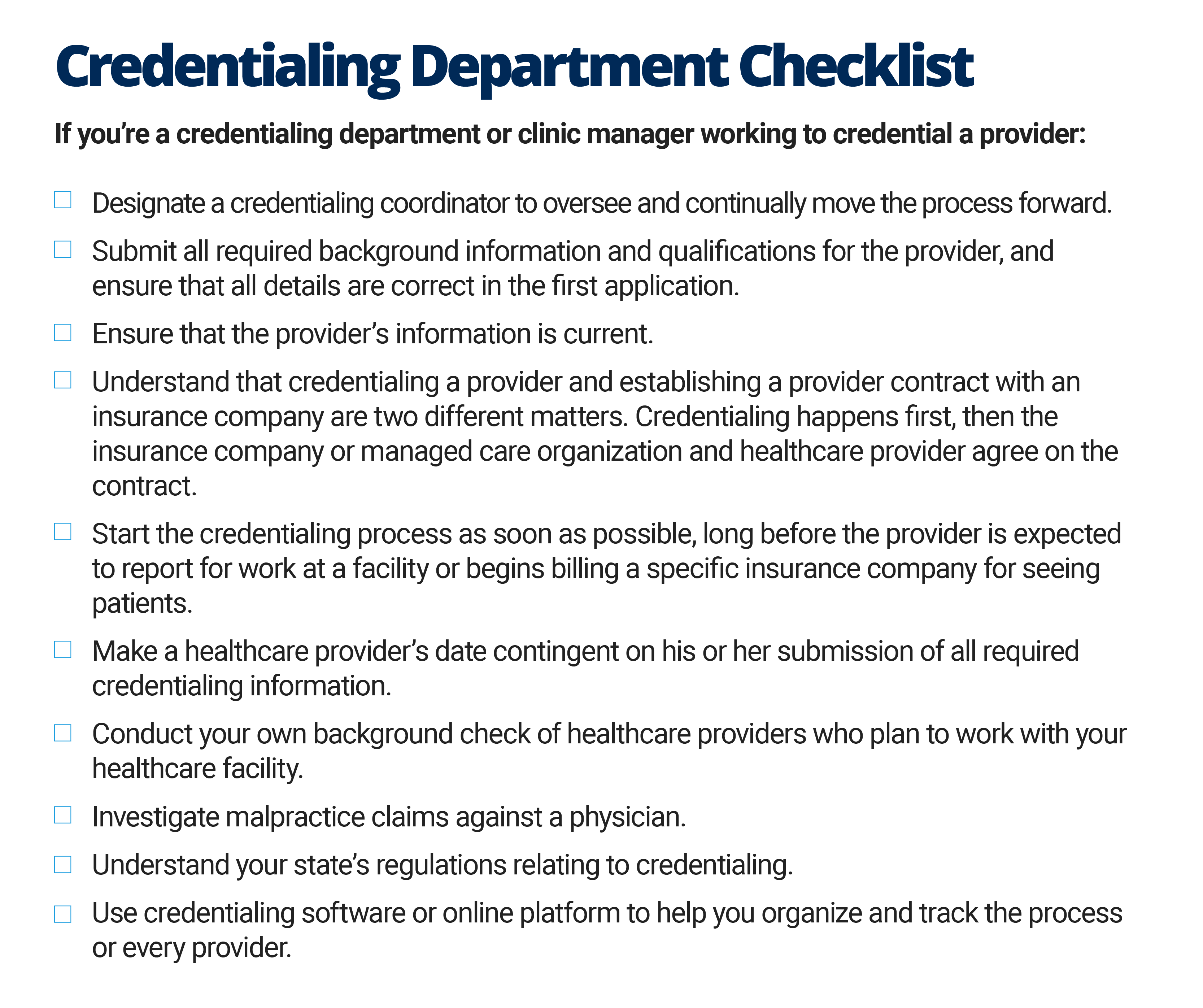
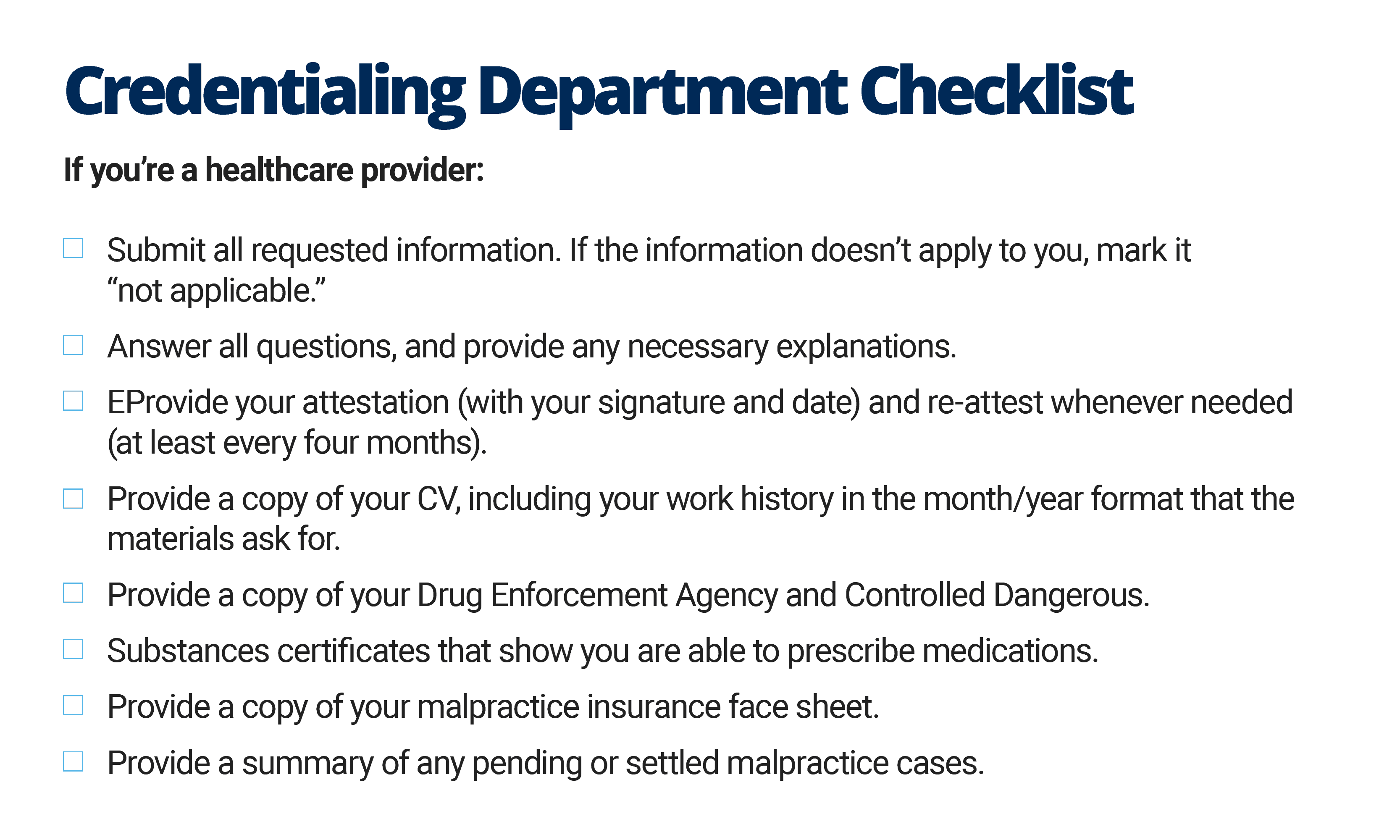 The Quick Guide To Healthcare Provider Credentialing Smartsheet
The Quick Guide To Healthcare Provider Credentialing Smartsheet
 Provider Enrollment Credentialing
Provider Enrollment Credentialing
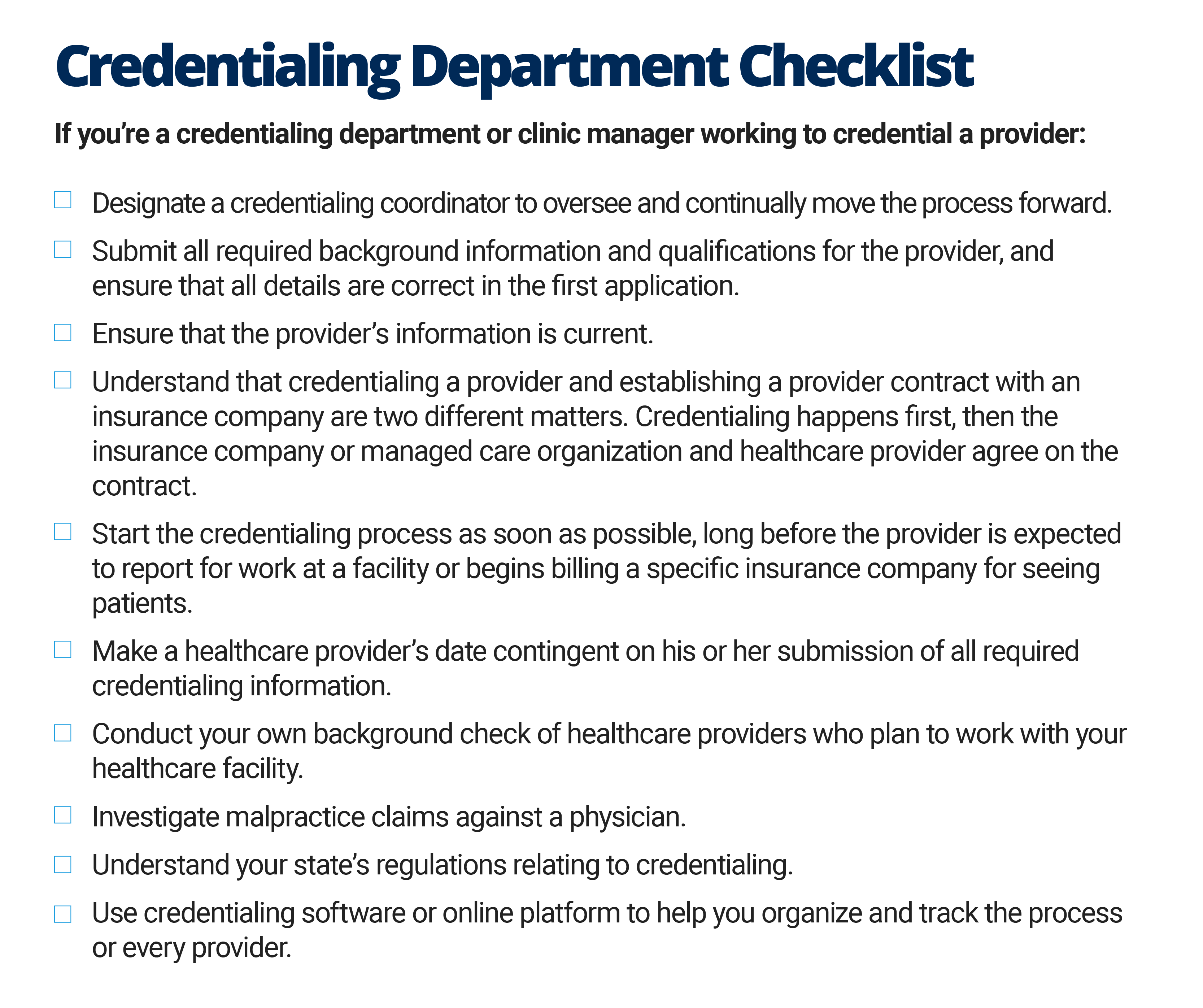 The Quick Guide To Healthcare Provider Credentialing Smartsheet
The Quick Guide To Healthcare Provider Credentialing Smartsheet
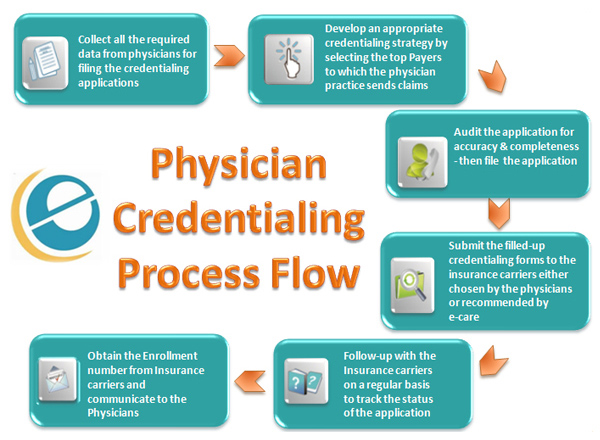 Physician Credentialing Provider Enrollment Services
Physician Credentialing Provider Enrollment Services
 Medical Provider Credentialing Service Credentialing Physician
Medical Provider Credentialing Service Credentialing Physician
Credentialing Expertise For Medical Professionals Addval Inc
 Medical Credentialing Med Advantage
Medical Credentialing Med Advantage
 Provider Enrollment And Credentialing Services Access Healthcare
Provider Enrollment And Credentialing Services Access Healthcare
 Credentialing Or Enrollment Mms Group
Credentialing Or Enrollment Mms Group
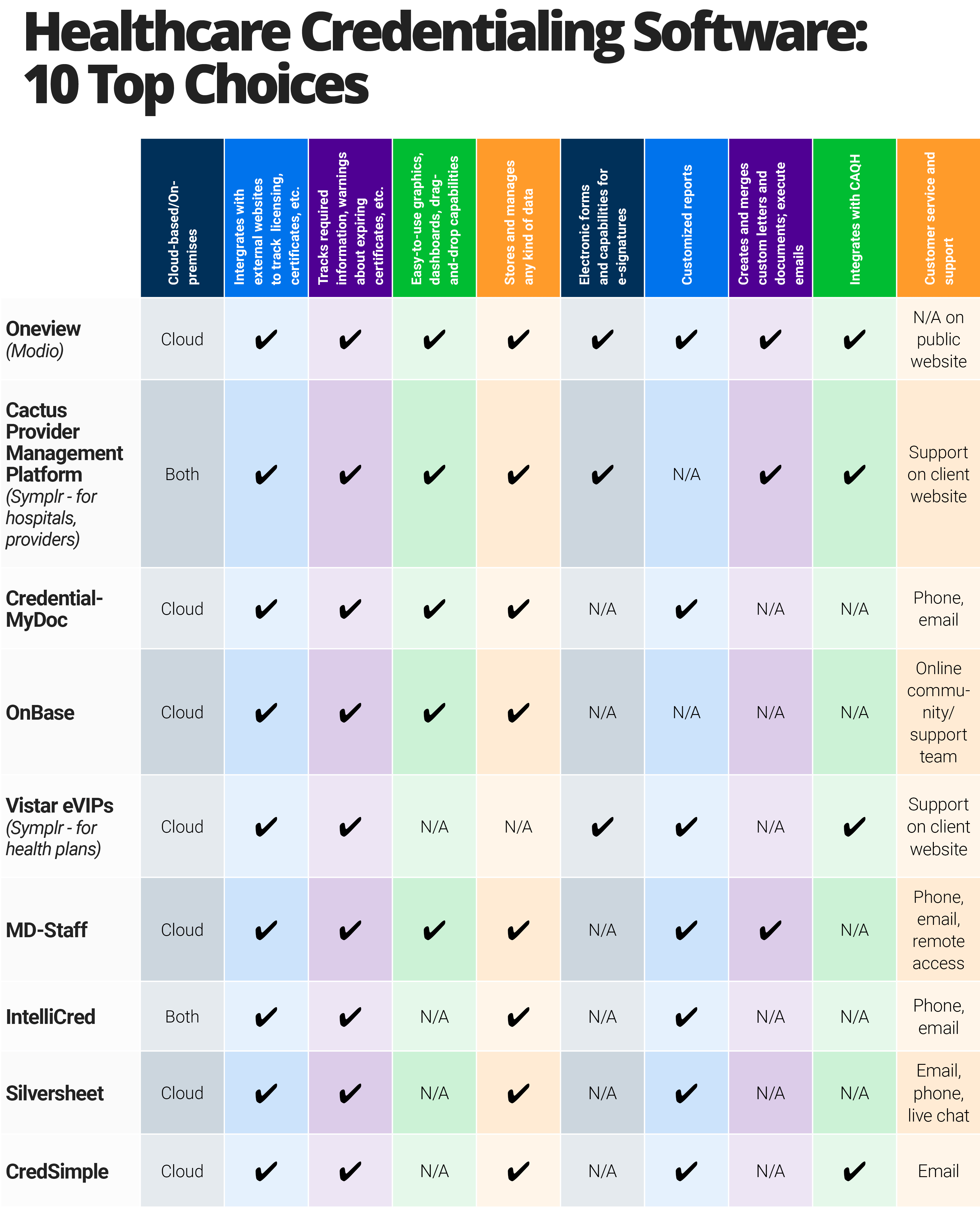 How To Choose Healthcare Credentialing Software Smartsheet
How To Choose Healthcare Credentialing Software Smartsheet
 Provider Credentialing Request Form
Provider Credentialing Request Form
Credentialing Legacy Consulting Services
 Credentialing Made Paperless At Molina Healthcare Laserfiche Solution Exchange
Credentialing Made Paperless At Molina Healthcare Laserfiche Solution Exchange
Comments
Post a Comment