Featured
What Does Out Of Network Mean For Health Insurance
Murat sarica Getty Images. This means medical providers may charge the full amount for your treatment and your insurance provider may not pay for these charges leaving the full burden of payment up to you.
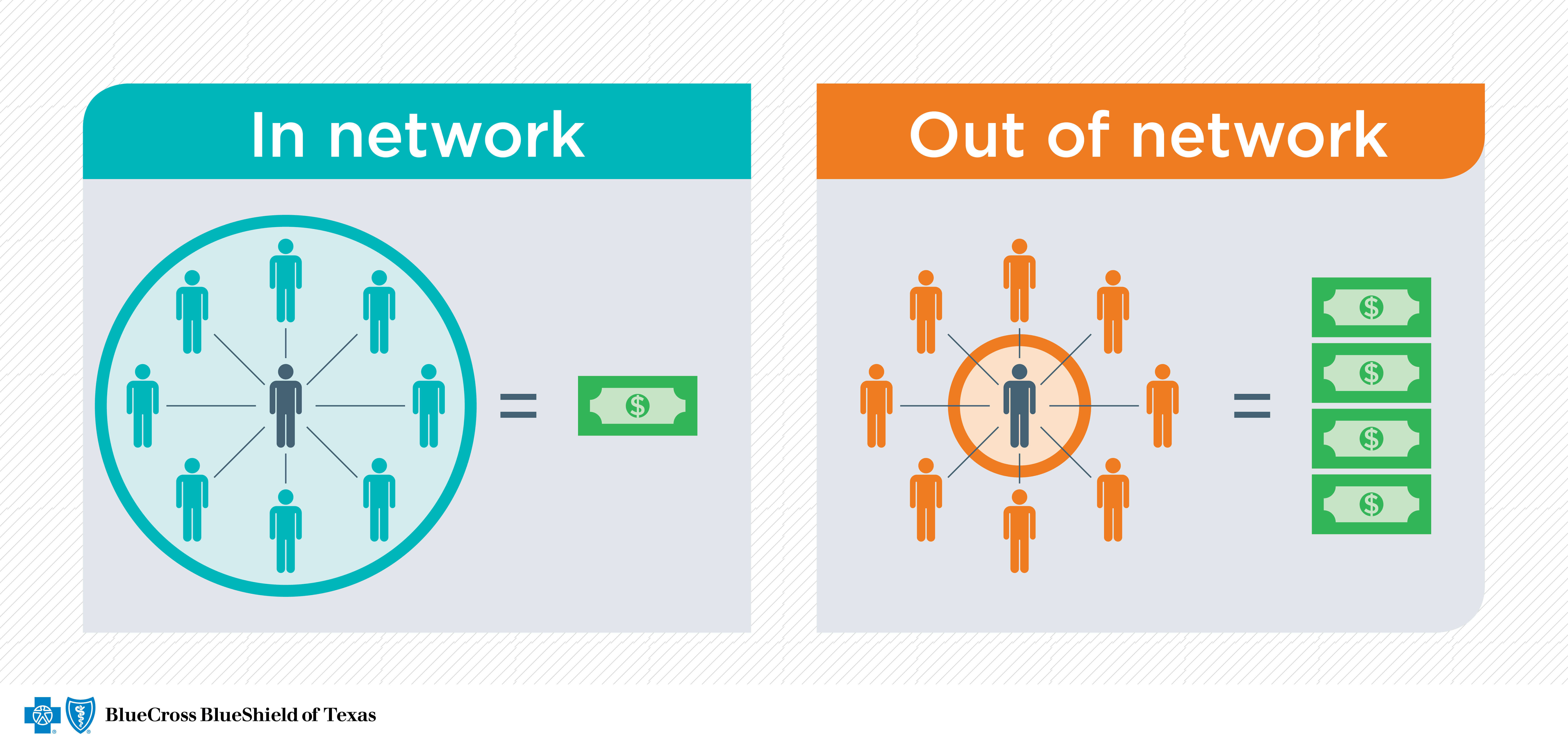 Check Provider Networks Before You Get Care Blue Cross And Blue Shield Of Texas
Check Provider Networks Before You Get Care Blue Cross And Blue Shield Of Texas
Lets say your out-of-network deductible is 1000 and your insurance company pays for 100 of services after you meet that amount.
What does out of network mean for health insurance. Out-Of-Network The term network doesnt just refer to your office computers. Your insurance company also has a network. That means youll have to pay 1000 out of pocket after which youll have met your.
Some health plans such as an HMO plan will not cover care from out-of-network providers at all except in an emergency. Help Protect You Your Family When Moving Abroad. This phrase usually refers to physicians hospitals or other healthcare providers who do not participate in an insurers provider network.
We also call them participating providers. A group of healthcare providers with whom it contracts to provide you service. While insurance companies may have some out-of-network benefits medical care from an out-of-network provider will usually cost more out-of-pocket than an in-network provider.
Keep an eye out for these terms. An-out-of-network care provider is one who hasnt agreed to participate with your insurer or accept the negotiated rates your insurer pays for a particular medical service. Back to Glossary Index.
Access High Levels of Medical Cover in the UK Abroad. Access High Levels of Medical Cover in the UK Abroad. Conversely in-network means that your provider has negotiated a contracted rate with your health insurance company.
Get a Personalised Quote. What does out of network mean. Updated on February 15 2020.
Your insurance company has agreed to pay 170 for that office visit. Annonce Private International Health Cover. We still pay 140 but youll be responsible for the remainder which is 110.
If you use an out-of-network provider health care services could cost more since the provider doesnt have a pre-negotiated rate with your health plan. If you have good out-of-network benefits your insurance company may reimburse you as much as 80 of each session fee depending on your plan and the therapists rate. This means that in some situations using your out-of-network benefits can actually be more affordable or comparable to your standard copay to see an in-network therapist.
Out of network simply means that the doctor or facility providing your care does not have a contract with your health insurance company. You can be charged with out-of-network costs when care is provided and the medical provider has not agreed to a negotiated fee with your insurance provider. Out-of-network coinsurance usually costs you more than in-network coinsurance.
This can sometimes result in higher prices. This is the amount of money you have to pay before you are eligible for reimbursement. This means that the provider has not signed a contract agreeing to accept the insurers negotiated prices.
In contrast Out-of-network health care providers do not have an agreement with your insurance company to provide care. Annonce Private International Health Cover. Out of network is a health insurance term that refers to health care providers not contracted with the insurer to provide health services at a negotiated rate.
When you go to a doctor or provider who doesnt take your plan we say theyre out of network. Get a Personalised Quote. Out-of-network refers to a health care provider who does not have a contract with your health insurance plan.
If you see a doctor or other provider that is not covered by your health insurance plan this is called out of network and you will have to pay a larger portion of your medical bill or all of it even if you have health insurance. Out-of-Network Coinsurance The percentage for example 40 you pay of the allowed amount for covered health care services to providers who dont contract with your health insurance or plan. Therefore a patient who sees an out-of-network provider can expected to pay much more than if they were to see an in-network provider.
Out of network simply means that the doctor or facility providing your care does not have a contract with your health insurance company. Or depending on your health plan the health care services. Help Protect You Your Family When Moving Abroad.
Or depending on your health plan the health care services may not be covered at all. If a provider is out-of-network this means they are not contracted with your insurance agency. When a doctor hospital or other provider accepts your health insurance plan we say theyre in network.
Out-of-network means that a doctor or physician does not have a contract with your health insurance plan provider. Some out-of-network providers choose to avoid contracting with insurance companies altogether and others may only select certain insurances they want to.
 What Does Out Of Pocket Mean In Health Insurance
What Does Out Of Pocket Mean In Health Insurance
 Ask Christina What Is The Difference Between In Network And Out Of Network Nerdwallet
Ask Christina What Is The Difference Between In Network And Out Of Network Nerdwallet
 Ppo Vs Hmo Insurance What S The Difference Medical Mutual
Ppo Vs Hmo Insurance What S The Difference Medical Mutual
 In Network Healthcare Providers Vs Those Who Accept Your Insurance What S The Difference Legacy Er
In Network Healthcare Providers Vs Those Who Accept Your Insurance What S The Difference Legacy Er
/Health-insurance-5687e75d5f9b586a9e4dd055.jpg) Dealing With Out Of Network Healthcare Bills
Dealing With Out Of Network Healthcare Bills
 Understanding The Difference Between In Network And Out Of Network Provider Coverage
Understanding The Difference Between In Network And Out Of Network Provider Coverage
 What Is A Ppo About Ppo Health Insurance Medical Mutual
What Is A Ppo About Ppo Health Insurance Medical Mutual
 In Network Vs Out Of Network What Does Out Of Network Mean
In Network Vs Out Of Network What Does Out Of Network Mean
 What Are Health Insurance Networks
What Are Health Insurance Networks
/health-insurance-card-56a695705f9b58b7d0e3b3ca.jpg) What An Out Of Network Provider Means
What An Out Of Network Provider Means
3 Things To Consider When Signing Up For Health Insurance
Health Insurance Network Types What Are Hmos And Ppos
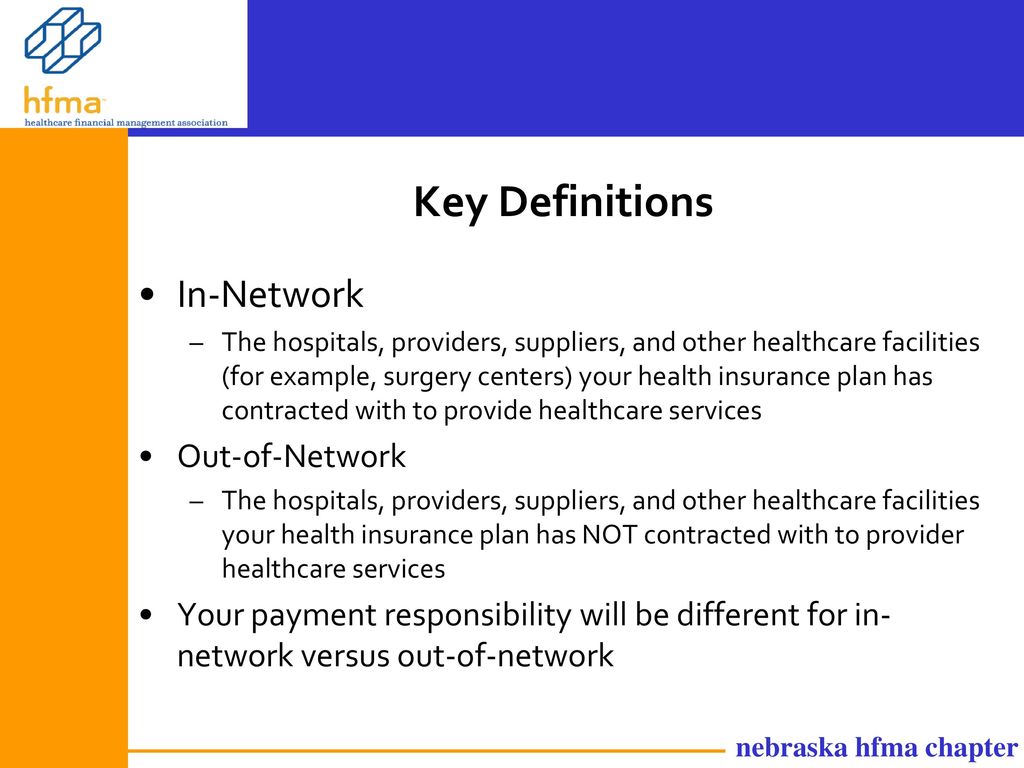 Health Insurance Key Definitions Frequently Asked Questions Ppt Download
Health Insurance Key Definitions Frequently Asked Questions Ppt Download
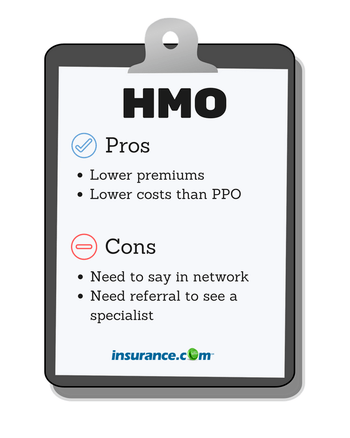 Hmo Vs Ppo Vs Other Plans What S The Difference Insurance Com
Hmo Vs Ppo Vs Other Plans What S The Difference Insurance Com
Comments
Post a Comment