Featured
Bcbs Federal Prior Authorization Form For Medication
Simply click on the form name to open them. First the request must come from a medical doctor.
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
If your office or facility has never used Provider Secured Services.

Bcbs federal prior authorization form for medication. The below forms are available for providers that are unable to submit a preauthorization online through NaviNet. Certain medical services and treatments need approval before you receive care. Medicaid only BCCHP and MMAI Medicaid Service Authorization Dispute Resolution Request Form.
Drugs included in our Prior Authorization Program are reviewed based on medical necessity criteria for coverage. Medical Transport Prior Approval Request. MASSACHUSETTS STANDARD FORM FOR MEDICATION PRIOR AUTHORIZATION REQUESTS Some plans might not accept this form for Medicare or Medicaid requests.
Certain drugs require prior authorization because Part D coverage of these drugs is available only if coverage is not available under Part B. Medicaid Claims Inquiry or Dispute Request Form. See the CMS Coverage database at.
Prior authorization is required for some membersservicesdrugs before services are rendered to confirm medical necessity. Bowel Prep Cost Share Reduction updated 100716. We review them to ensure they are medically necessary.
Prior Authorization requirements may vary. If you have questions or concerns regarding these programs please call Prime Therapeutics at 800-289-1525. Prior Authorization Step Therapy Formulary Exception.
Blue Cross Federal Employee Program Use these forms to obtain prior authorization for administering medications in physicians offices and outpatient hospitals including urgent care hospital-based infusion care centers and clinics where the drug is injected or infused and billed on a UB04 or CMS 1500 form. Blue Cross Blue Shield of Arizona Mail Stop A115 PO. Forms to Download PDF format The forms below are all PDF documents.
Box 13466 Phoenix AZ 85002-3466 Page 1 of 2 Member Information. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan.
Non-Network Provider Written Direction of Payment Form. GENERAL PRESCRIPTION DRUG COVERAGE AUTHORIZATION REQUEST FORM This form is for authorization of prescription drug benefits only and must be COMPLETELY filled out. This is called prior approval precertification or preauthorization.
Medicaid only BCCHP and MMAI. This form is being used for. Floor Prior Auth Dept 200 Stevens Drive Philadelphia PA 19113.
Authorized Representative Designation Form. 81 rows Drug Prior Authorization Request Forms. We offer these convenient options.
Step Therapy Program Criteria Summary and Fax Form List. You can find detailed instructions on how to file an appeal in the Disputed Claims Process document. GENERAL INFORMATION Patient Name Request Type please check one Prior Authorization Step Therapy Exception Request for Quantity Limit Exception City Appeal Mandatory Generic.
Submit a Pharmacy Pre-Authorization Online. Actemra IV Actemra SC. When you request prior authorization from us we want the process to be fast easy and accurate.
Form Title Networks Expedited Pre-service Clinical Appeal Form. Use this form to select an individual or entity to act on your behalf during the disputed claims process. Pharmacy Prior Authorization Request Form Do not copy for future use.
Submit the completed form. Prior authorization sometimes called preauthorization or pre-certification is a pre-service utilization management review. _____ _____ Part D vs.
Medical Forms Resource Center MFRC This online tool makes it easy to submit prior authorization requests for certain services. Youll need to sign up. Blue Cross Completes prior authorization criteria for a brand-name DAW.
Attention Pharmacy at 1-855-811-9326 By mail. Step Therapy Program Criteria Summary and Fax Form List. The doctor can practice in an office or a facility.
If you do not obtain prior approval there may be a reduction or denial of your benefit. What other drugs if any has the patient taken in the past for this condition and what was the patients response. Durable Medical Equipment Certification Form.
What you need to request medical drug authorization. The tool guides you through all of the forms you need so you can. This article has the instructions and forms.
If you have questions or. Office notes labs and medical testing relevant to the request that show medical justification are required. Forms are updated frequently.
Drugs with step therapy requirements may be covered if a prior health plan paid for the drug documentation of a paid claim may be required. Medication Prior Authorization Request Confidential Information June 2020 PH-ANR-25Rev070120. Submit a Transplant Prior Authorization Request.
Initial Request C o n tinua R ewal R ques Reason for request check all that apply. Review the prior authorizationstep therapy program overview list to help you determine which prior authorization form is used for the medication being prescribed. Then youll need access to to Provider Secured Services.
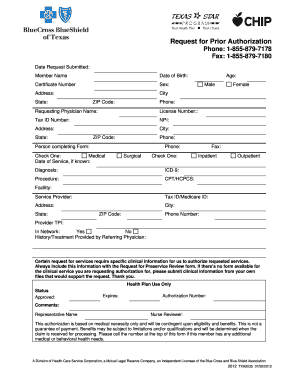 Fillable Online Bcbs Request For Prior Authorization Form Fax Email Print Pdffiller
Fillable Online Bcbs Request For Prior Authorization Form Fax Email Print Pdffiller
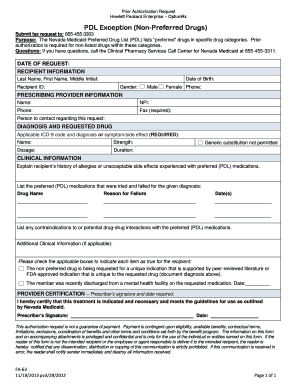
Https Www Empireblue Com Provider Noapplication F3 S2 T2 Pw Ad067834 Pdf Refer Ehpprovider
Https Member Carefirst Com Carefirst Resources Pdf Non Formulary Drug Exception Form Pdf
Https Www Bcbsvt Com Sites Default Files 2020 02 2020 Fep Blue Focus Pa List 12 18 19 Pdf
 Highmark Bcbs Medication Prior Authorization Form Best Of Anthem Express Scripts Prior Authorization Form New Free Gov Forms Models Form Ideas
Highmark Bcbs Medication Prior Authorization Form Best Of Anthem Express Scripts Prior Authorization Form New Free Gov Forms Models Form Ideas
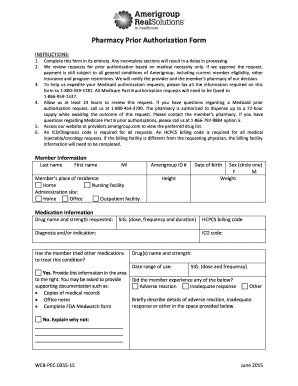
 Regence Prior Authorization Form For Medication Fill Online Printable Fillable Blank Pdffiller
Regence Prior Authorization Form For Medication Fill Online Printable Fillable Blank Pdffiller
Https Www Blueshieldca Com Bsca Bsc Public Common Portalcomponents Provider Streamdocumentservlet Filename Prv Fep Medical Injectable Drug Pdf
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
 30 Printable Blue Cross Blue Shield International Medical Claim Form Templates Fillable Samples In Pdf Word To Download Pdffiller
30 Printable Blue Cross Blue Shield International Medical Claim Form Templates Fillable Samples In Pdf Word To Download Pdffiller
 Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Https Www Anthem Com Provider Noapplication F0 S0 T0 Pw E221326 Pdf Na Pharminfo
Https Www Mybcbswny Com Stateplans Nyny Nyw Priorauthforprescriptions Pdf
Https Providers Bcbsal Org Portal Documents 10226 301829 General Prescription Drug Coverage Authorization Request Form A9b9b8bf 922b 469a B21f E396da68c634 Version 1 5
 Regence Prior Authorization Form For Medication Fill Online Printable Fillable Blank Pdffiller
Regence Prior Authorization Form For Medication Fill Online Printable Fillable Blank Pdffiller
Comments
Post a Comment