Featured
- Get link
- X
- Other Apps
Anthem Bcbs Prior Authorization
Rocky Mountain Hospital and Medical Service Inc. Anthem Blue Cross and Blue Shield Anthem may request specific additional information upon review of the request for prior authorization.
 Anthem Blue Cross Prior Authorization Form Fax Number Brilliant Tricare Prior Auth Form Forms Employee Gateway Express Scripts Prior Models Form Ideas
Anthem Blue Cross Prior Authorization Form Fax Number Brilliant Tricare Prior Auth Form Forms Employee Gateway Express Scripts Prior Models Form Ideas
Anthem Health Plans Inc.

Anthem bcbs prior authorization. Select the Drug List Search tab to access up-to-date coverage information in your drug list including details about brands and generics dosagestrength options and information about prior authorization of your drug. Prior Authorization Requirements HealthKeepers Inc. Inside Los Angeles County.
After hours verify member eligibility by calling the 247 NurseLine at 1-800-224-0336. Georgia Local PrecertificationPrior Authorization List Updated. - Anthem working with Optum to collect medical records for Medicare Risk Adjustment MRA - Helping our senior members.
Please check your schedule of benefits for coverage information. Use the Prior Authorization Lookup Tool within Availity or. Please fill out the Prescription Drug Prior Authorization Or Step Therapy Exception Request Form and fax it to 877 327-8009.
Blue Cross Blue Shield Healthcare Plan of Georgia Inc. 010120 19325 Mammaplasty Augmentation. Services Requiring Prior Authorization The table below outlines the services that require Prior Authorization PA for Anthem Blue Cross Medicaid Business members enrolled in Medi-Cal Managed Care Healthy Families Program HMO and EPO Access for Infants and Mothers AIM Program HMO and EPO and Major Risk Medical Insurance Program MRMIP.
Please check your schedule of benefits for coverage information. 1 day agoAnthem hopes the information exchange partnership will help automate prior authorization requests provide data-driven insights into patient care and promote value-based payments. Contact the Customer Care Center.
This approval process is called prior authorization. The Colorado Prescription Drug Prior Authorization Request formmay be used to submit prior authorization PA requests for members enrolled in a Colorado health plan regardless of residenceThe preferred method to submit PA. ICR offers a fast efficient way to securely submit prior authorization requests with clinical documentation.
Anthem Blue Cross is the trade name of Blue Cross of California and Anthem Blue Cross Partnership Plan is the trade name of Blue Cross of California Partnership Plan Inc. WProsthetic Implant Anthem SURG00023 19328 Removal Intact Mammary Implant Anthem SURG00023 19330 Removal Mammary Implant Matl Anthem SURG00023 19340 Immediate Insertion Breast Prosthesis Following Mastopexy MastectomyIn Reconstruction. Customer Care Center hours are Monday to Friday 7 am.
The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. Drug listFormulary inclusion does not infer a drug is a covered benefit. Reimbursement Policy Definitions A-Z.
Our Interactive Care Reviewer ICR tool via Availity is the preferred method for submitting prior authorization requests offering a streamlined and efficient experience for providers requesting inpatient and outpatient medical or behavioral health. For the member to receive maximum benefits Anthem must authorize the services for which. Attention prescribing providers with members enrolled in an Anthem Colorado health plan.
Anthem Blue Cross and Blue Shield is the trade name of. To request or check the status of a prior authorization request or decision for a particular plan member access our Interactive Care Reviewer ICR tool via Availity. Prior Authorization Lookup Tool.
Browse commonly requested forms to find and download the one you need for various topics including pharmacy enrollment claims and more. Outside Los Angeles County. Once logged in select Patient Registration Authorizations Referrals then choose Authorizations or AuthReferral Inquiry as.
Anthem Blue Cross Anthem is available by fax or Interactive Care Reviewer ICR 247 to accept prior authorization requests. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. New prior authorization requirements for providers may apply for new or updated reimbursement policies medical policies or prior authorization requirements.
PrecertificationPrior authorization is the determinationby Anthem that selected inpatient and outpatient medical services including surgeries major diagnostic procedures and referrals are medically necessary. HMO products underwritten by HMO Colorado Inc. AIM Specialty Health is an independent company providing some utilization review services on behalf of Anthem Blue Cross.
Recommends submitting prior authorization requests for Anthem HealthKeepers Plus members via Interactive Care Reviewer ICR a secure Utilization Management tool available in Availity. Download forms guides and other related documentation that you need to do business with Anthem. The Colorado Prescription Drug Prior Authorization Request formmay be used to submit prior authorization PA requests for.
Independent licensees of the. Attention prescribing providers with members enrolled in an Anthem Colorado health plan.
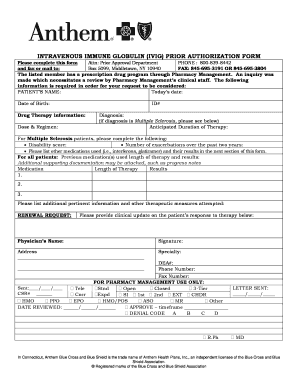
 Fillable Online Anthem Prior Authorization Form For Procedures Fax Email Print Pdffiller
Fillable Online Anthem Prior Authorization Form For Procedures Fax Email Print Pdffiller
 Fillable Online Anthem Prior Auth Request For Form Fax Email Print Pdffiller
Fillable Online Anthem Prior Auth Request For Form Fax Email Print Pdffiller
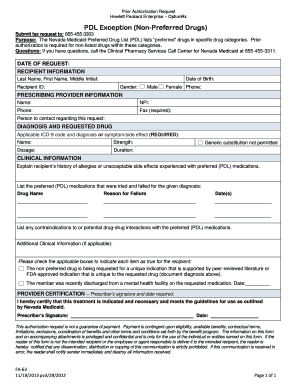 2012 Form Nv Fa 63 Fill Online Printable Fillable Blank Pdffiller
2012 Form Nv Fa 63 Fill Online Printable Fillable Blank Pdffiller
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
Https Mss Anthem Com California Mmp Caca Mmp 2020coveragedeterminationform Eng Pdf
 Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Https Www11 Anthem Com Ca Provider F1 S0 T0 Pw E229275 Pdf Refer Provider
 Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
 Anthem Blue Cross Medi Cal Prior Authorization Form Lovely Optum Rx Prior Authorization Form Templates Optumrx Best Hello Models Form Ideas
Anthem Blue Cross Medi Cal Prior Authorization Form Lovely Optum Rx Prior Authorization Form Templates Optumrx Best Hello Models Form Ideas
Https Www Anthem Com Provider Noapplication F1 S0 T0 Pw Ad080665 Pdf Refer Ahpprovider
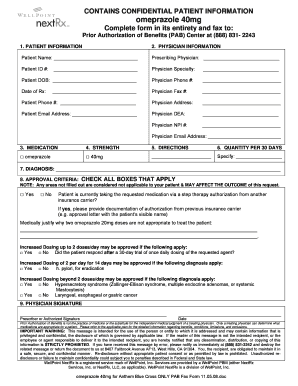
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Https Www Anthem Com Provider Noapplication F4 S6 T0 Pw E213404 Pdf Refer Ahpprovider State Ct
Https Www Anthem Com Provider Noapplication F0 S0 T0 Pw E228625 Pdf Na Pharminfo
 Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
Comments
Post a Comment